Bentall De Bono surgery using a composite graft containing a biological prosthesis of the aortic valve under artificial circulation: A clinical case study
CASE REPORT
Bentall De Bono surgery using a composite graft containing a biological prosthesis of the aortic valve under artificial circulation: A clinical case study
Article Summary
- DOI: 10.24969/hvt.2024.517
- CARDIOVASCULAR DISEASES
- Published: 02/10/2024
- Received: 12/11/2023
- Revised: 07/09/2024
- Accepted: 08/09/2024
- Views: 4645
- Downloads: 2537
- Keywords: Cardiac surgery, Bentall De Bono method, bicuspid aortic valve, biological valve
Address for Correspondence: Jamal I. Ashimov, DOC CARDIO Center Salymbekov University, Bishkek, Kyrgyzstan,
Email: transplant@mail.ru
1B.K. Kadyraliev, 1V.B.Arutyunyan, 1A.A. Alexandrov 2Jamal I. Ashimov, 2A.B.Zhumanazarov, 2Janybek J. Gaybildaev, 2Ruslan A. Sadabaev, 3Zhakshylyk Abdimitalip Uulu, 2A.T.Satybaldiev, 3T.J.Duishoev, 2A. Kurmanbekova
1Federal Center of Cardiovascular Surgery named after S.G. Sukhanov, Perm, Russia
2DOC CARDIO Center Salymbekov University, Kyrgyzstan, Bishkek
3Medical Center "Cardio-Asia Plus", Kyrgyzstan, Osh
Abstract
Objective: The aim of our article is to report the positive outcome of the prosthetic biological aortic valve replacement of using Bentall De Bono procedure under artificial circulation.
Case presentation: A male patient, born in 1954, was admitted to our clinic with complaints of marked dyspnea and weakness at the slightest physical load, accompanied by heart palpitations. The patient had a history of congenital heart defect, namely bicuspid aortic valve. His condition had been deteriorating since August 2023, with symptoms of heart failure, pleural effusion and hepatomegaly. Evacuation of pleural effusion was repeatedly performed. On further examination, echocardiography revealed marked atheromatous of the ascending aorta. Aneurysm of the ascending aorta, dilatation of the aortic root, annuloaortic ectasia of the bicuspid aortic valve. Aortic regurgitation of the 2nd degree. Mitral regurgitation of the 2nd degree. On chest computed tomography, the heart was normally located, minimal accumulation of effusion up to 4.0 mm was noted in the pericardial cavity. The aorta was located typically, the diameter of the ascending section was up to 63 mm, aortic arch up to 42 mm, descending aorta up to 27 mm, the contours were clear, no wall thickening was noted. Bentall De Bono method surgery was performed using a biological valve under artificial circulation and hemodynamic support. The patient was discharged on the 10th day after the operation, only insignificant mitral insufficiency was noted on control echocardiography.
Conclusion: Bentall De Bono operation using a biological prosthesis is the most justified treatment tactic if there is no history of rheumatic valve lesions.
Key words: Cardiac surgery, Bentall De Bono method, bicuspid aortic valve, biological valve
Introduction
"Gold standard" treatment of aortic root pathologies is Bentall-De Bono surgery with implantation of a composite graft containing a mechanical aortic valve prosthesis, which is used worldwide (1). Surgery of the aortic root, aortic valve and ascending aorta is one of the challenging operations in cardiovascular surgery. One of the effective surgical techniques is the Bentall-De Bono operation using a synthetic conduit containing a mechanical or biological prosthesis (2), which was first described in 1968 by Hugh Bentall and Anthony De Bono.
In the last decades, aortic surgery has thrived a number of changes and improvements, because aortic disease might cause life-threatening complications in the form of rupture or dissection, but current surgery allows complex, lengthy operations and minimizes risks (3, 4). Aortic valve lesions with dilated or dissected aortic root and ascending aorta are an absolute indication for aortic valve reconstruction. In addition, planned surgery is reasonable in the presence of significant dilation of the sinuses of Valsalva, sinotubular junction. Among the solutions for the complex aortic pathology, the most suitable is the method of Bentall-De Bono, who proposed a surgical reconstruction using a synthetic conduit containing a mechanical aortic prosthesis (5, 6). One of the disadvantages of this technique is the lifelong use of anticoagulant therapy in patients due to the maintenance of the synthetic conduit by the mechanical prosthesis.
To address this issue, cardiovascular surgery is undergoing a slight change; cardiac surgeons prefer valve-preserving surgery or the use of biological prostheses to avoid lifelong anticoagulant therapy.
Etz et al. (7) reviewed 275 patients who underwent aortic root reconstruction with a conduit containing a biological prosthesis. Hospital mortality was 17 patients, irreversible stroke occurred in 4 patients (1.5%), and only 1 patient underwent reoperation after 12 years due to insufficiency of the biological valve. One of the main complications of the postoperative period is structural dysfunction of the prosthesis, which requires repeated surgery to replace the prosthesis. The main disadvantage of this operation is the difficulty of isolated valve replacement and requires repeated aortic root prosthesis (8-10).
Albertini et al. (11) provided a modified surgical technique to simplify reoperation after biologic valve prosthesis in Bentall-De Bono surgery. This technique allows fixing the bioprosthesis in the inner part of the septic conduit, leaving more than 2 mm of free edge, forming a "skirt", subsequently the end of the skirt is fixed to the aortic fibrous ring, thus the distance between the fibrous ring and the biological valve is more than 2 mm, allowing further replacement of the bioprosthesis, leveling the complete replacement of the aortic root.
The aim of our article is to report the positive outcome of the prosthetic biological aortic valve replacement of using Bentall De Bono procedure under artificial circulation.
Case presentation
A male patient, born in 1954, height 183 cm and weight 92.5 kg, was admitted to our clinic with complaints of marked dyspnea and weakness at the slightest physical exertion, accompanied by heart palpitations and sleep disturbance.
The patient had a history of congenital heart disease, namely bicuspid aortic valve. His condition worsened since August 2023, with symptoms of heart failure, pleural effusion and hepatomegaly. Evacuation of pleural effusion was repeatedly performed. On further examination, echocardiography revealed marked atheromatous lesions in the ascending aorta, aneurysm of the ascending aorta, dilatation of the aortic root, annuloaortic ectasia of the bicuspid aortic valve. Hemodynamically significant aortic regurgitation of the 2nd degree. Mitral regurgitation of the 2nd degree. Left ventricular dilatation, moderate pulmonary hypertension. Left ventricular systolic function was satisfactory. The longitudinal function of the right ventricle was preserved. On computed tomography of the chest, the heart was normally located, minimal accumulation of effusion up to 4.0 mm was noted in the pericardial cavity. The aorta was typically located, the ascending aorta diameter was up to 63 mm, the aortic arch was up to 42 mm, the descending aorta was up to 27 mm, the contours were clear, and no wall thickening was noted (Fig. 1). The pulmonary trunk and pulmonary arteries were of normal diameters. No significant narrowing was noted on coronary angiography.
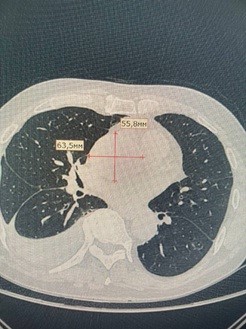
Figure 1. Computed tomography of the ascending part of the aorta (see explanation in text)
Taking into account all the above-mentioned complaints, the results of instrumental investigations, the patient's age, his tendency to choose a biological valve and the approval of the patient's relatives, a decision was made to perform Bentall De Bono operation using a biological valve.
Surgical access
We performed percutaneous thoracic incision, midline longitudinal sternotomy, and hemostasis. The pericardium was opened longitudinally, no pathologic fluid was found. There was aneurysmal dilation of the ascending aorta starting from the aortic root, 6.3-5.5 cm in diameter, tense, livid in places. The diameter of the aorta in the area of transition to the arch was about 4.2 cm. The aorta was isolated, taken for cicatricial sutures, heparin was infused. The aorta and right atrium were cannulated with a two-stage cannula, and artificial circulation was started. The upper right pulmonary vein was drained to decompress the left ventricle. The aorta was clamped closer to the brachycephalic trunk, and the aortic wall was opened longitudinally. The aortic wound was dilated, blood cardioplegia in the mouth of the left and right coronary arteries, cardiac arrest (Cardioplegia in the subsequent plan). The aneurysmal sac was dissected out. The aortic wall and coronary arteries at the site of dissection were dissected out. On the revision of the aortic root and aortic valve - the ring was dilated, the valve is bicuspid, the flaps are changed, the sinuses of Valsalva were dilated. The aortic wall was thinned, altered by atherosclerosis. The aortic valve was prosthetic with a biological prosthesis and the ascending part of the aorta by Bentall-De Bono method. Coronary artery bypass grafting into a conduit was performed (Fig. 2). Air embolism prophylaxis was applied. The aorta was released. There was a self-restoration of cardiac activity. There was insignificant blood flow from the anastomoses, requiring additional hemostatic sutures, and bleeding stopped. Hemodynamics stabilized, and artificial circulation was smoothly ended. After control hemostasis, myocardial electrodes to the right ventricle and right atrium were sutured. Decannulation. Protamine sulfate was injected. Drains were placed in the pericardial cavity, anterior mediastinum and right lung. We applied layer-by-layer suturing of the wound.
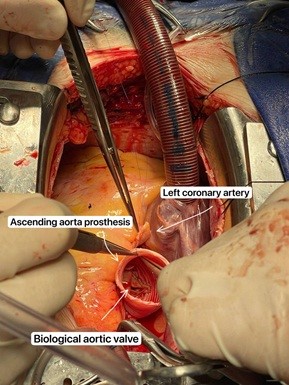
Figure 2. Stitching of the left coronary artery – intraoperative view
Postoperative period
The postoperative period proceeded smoothly without any major complications. The wound healed with primary tension. The patient's condition was satisfactory, with positive dynamics.
Control echocardiography on the 18th day after the operation showed that left ventricular systolic function was satisfactory. The longitudinal function of the right ventricle was satisfactory. No signs of pulmonary hypertension were observed on echocardiography.
Normal function of the valve-containing conduit in the aortic position was observed. On control radiography, we did not see any special changes in the respiratory system. Control laboratory examination showed a decrease in hemoglobin and hematocrit, a low international normalized ratio (INR) and a slight increase in renal tests, all of which were corrected and brought to normal values in further treatment. On the 10th day after the operation, the patient was discharged home in satisfactory condition, without major complications.
Discussion
Pantaleo et al. (12) compared the results of Bentall De Bono surgery using a classic mechanical valve and a modified biological valve. In their study, they included 1112 patients, divided them according to 29 parameters, used a statistical method, excluding systematic errors in the choice of treatment methods, and obtained 2 similar groups of 138 patients each. Their analysis showed that there was no particular difference in mortality between mechanical and biological valve in long-term follow-up (HR 0.88; 95% CI: 0.50-2.14; p 0.4). Only previous cardiac surgery was the significant predictor of late death (HR: 6.41; 95% CI: 1.41-29.48; p=0.02). Measures such as neurologic complication, myocardial infarction, renal failure, length of hospital stay, and hospital mortality were relatively identical between groups. The authors concluded that the Bio-Bentall procedure is a safe and effective treatment for aortic pathology. The choice between a biological and mechanical aortic valve did not particularly affect early and late adverse outcomes.
A 10-year follow-up by Byrne et al. (13) showed that the well-being of patients in both groups was similar, and they could find no particular significant differences with respect to early or late complications, complications with respect to valve type, and overall mortality. Independent predictors of late patient death were concomitant coronary artery surgery, valve repeated prosthesis, perioperative stroke and patient age, but not type of conduit and all of these were confirmed by multivariate analyses (13).
Briefly, we note the priorities for choosing a biological valve over a mechanical valve in the Bentall De Bono procedure and beyond. One important aspect is that the biological valve reduces the long-term use of anticoagulant agents than the mechanical valve. This reduces the risk of thrombosis and bleeding, especially important for individuals at high risk of traumatic injury, for women who intend to have children and for elderly individuals who tend to be forgetful or have certain memory lapses. Patients with a biological valve are allowed to lead a more active and less restricted lifestyle. Since there is less constant monitoring of blood clotting and anticoagulant medication, which is characteristic of the mechanical valve.
Not an unimportant aspect is the presence of noise from the operation of the mechanical valve after prosthetics. It is characteristic for persons susceptible to different types of noise. Because of the constant presence of noise when closing the prosthesis, patients developed various types of psychological disorders, thus worsening the quality of life (14).
As a result, we are inclined to believe that the biological valve should be the priority in choosing the type of valve. Thus, the popularization of such operations will improve the results of surgical treatment of this category of patients and their quality of life.
Ethics: Informed consent was obtained from the patient before all procedures.
Peer-review: External and Internal
Conflict of interest: None to declare
Authorship: B.K.K., V.B.A., A. A.A., J.I.A., A.B.Zh, J.J.G, R.A.S., Zh.A.u., A.T.S., T.J.D., and A.K.
equally contributed to management of patient and manuscript preparation, and fulfilled authorship criteria.
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: We declare that we did not use AI-assisted technologies in preparation of this manuscript
References
| 1.Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax 1968; 23: 338-9. Doi: 10.1136/thx.23.4.338 https://doi.org/10.1136/thx.23.4.338 |
||||
| 2.Urbanski P.P. Replacement of the ascending aorta and aortic valve with a valved stentless composite graft. Ann Thorac Surg 1999; 67: 1501-2. Doi: 10.1016/s0003- 4975(99)00184-8 https://doi.org/10.1016/S0003-4975(99)00184-8 |
||||
| 3.Detter C, Mair H, Klein HG, Georgescu C, Welz A, Reichart B. Long-term prognosis of surgically-treated aortic aneurysms and dissections in patients with and without Marfan syndrome. Eur J Cardiothorac Surg 1998; 13: 416-23. https://doi.org/10.1016/S1010-7940(98)00043-8 |
||||
| 4.Lepore V, Larsson S, Bugge M, Mantovani V, Karlsson T. Replacement of the ascending aorta with composite valve grafts: long term results. J Heart Valve Dis 1996; 5: 240-6. | ||||
| 5.Kouchoukos NT, Wareing TH, Murphy SF, Perrillo JB. Sixteen-year experience with aortic root replacement. Results of 172 operations. Ann Surg 1991; 214: 308-18. https://doi.org/10.1097/00000658-199109000-00013 |
||||
| 6.Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax 1968; 23: 338-9. https://doi.org/10.1136/thx.23.4.338 |
||||
| 7.Etz CD, Homann TM, Rane N, Bodian CA, Di Luozzo G, Plestis KA, et al. Aortic root reconstruction with a bioprosthetic valved conduit: a consecutive series of 275 procedures. J Thorac Cardiovasc Surg 2007; 133:1455-63. Doi: 10.1016/j.jtcvs.2007.01.058 https://doi.org/10.1016/j.jtcvs.2007.01.058 |
||||
| 8.Kirsch EWM, Radu NC, Mekontso-Dessap A, Hillion ML, Loisance D. Aortic root replacement after previous surgical intervention on the aortic valve, aortic root, or ascending aorta. J Thorac Cardiovasc Surg 2006; 131: 601-8. . doi: 10.1016/j.jtcvs.2005.11.007 https://doi.org/10.1016/j.jtcvs.2005.11.007 |
||||
| 9.Joudinaud T.M., Baron F., Raffoul R., Pagis B., Vergnat M., Parisot C., et al. Redo aortic root surgery for failure of an aortic homograft is a major technical challenge. Eur J Cardiothorac Surg 2008; 33: 989-94. Doi: 10.1016/j.ejcts.2008.01.054 https://doi.org/10.1016/j.ejcts.2008.01.054 |
||||
| 10.Liu C, Doig F, Naidoo R Tesar P. Redo aortic valve replacement following Bio-Bentall's procedure. Heart Lung Circ 2019; 28: e131-3. doi: 10.1016/j.hlc.2019.04.015 https://doi.org/10.1016/j.hlc.2019.04.015 |
||||
| 11.Albertini A, Dell'Amore A, Zussa C, Lamarra M. Modified Bentall operation: the double sewing ring technique. Eur J Cardiothorac Surg 2007; 32: 804-6. Doi: 10.1016/j.ejcts.2007.07.011 https://doi.org/10.1016/j.ejcts.2007.07.011 |
||||
| 12.Pantaleo A, Murana G, Di Marco L, Jafrancesco G, Barberio G, Berretta P, et al. Biological versus mechanical Bentall procedure for aortic root replacement: a propensity score analysis of a consecutive series of 1112 patients. Eur J Cardiothorac Surg 2017; 52: 143- 9. Doi: 10.1093/ejcts/ezx070 https://doi.org/10.1093/ejcts/ezx070 |
||||
| 13. Byrne JG, Gudbjartsson T, Karavas AN, Mihaljevic T, Phillips BJ, et al. Biological vs. mechanical aortic root replacement Eur J Cardio-Thorac Surg 2003; 23: 305-10. Doi: 1016/s1010-7940(02)00816-3 https://doi.org/10.1016/s1010-7940(02)00816-3 |
||||
| 14. Huang JS, Hong ZN, Sun KP, Cao H, Chen Q. Effect of the different mechanical mitral valve sounds on the patients' quality of life. Thorac Cardiovasc Surg 2020; 68: 492-7. Doi: 10.1055/s-0039-1695788 https://doi.org/10.1055/s-0039-1695788 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

