Hybrid treatment of a saccular aneurysm of the aortic arch - long term follow-up: A case report
CASE REPORT
Hybrid treatment of a saccular aneurysm of the aortic arch - long term follow-up: A case report
Article Summary
- DOI: 10.24969/hvt.2024.520
- CARDIOVASCULAR DISEASES
- Published: 11/10/2024
- Received: 28/08/2024
- Revised: 29/09/2024
- Accepted: 03/10/2024
- Views: 3987
- Downloads: 2610
- Keywords: Aneurysm, aortic arch, hybrid repair, TEVAR, Chimney technique
Address for Correspondence: Fabio Massimo Oddi, Vascular Surgery Unit, Department of Biomedicine and Prevention, University of Rome Tor Vergata, Rome, Italy
Email: Fabio.Massimo89@gmail.com Phone: +390620902833
ORCID: Fabio Massimo Oddi - 0000-0001-8081-807X, Arnaldo Ippoliti - 0000-0001-5311-8203
Fabio Massimo Oddi, Grazia Granata, Mauro Fresilli, Martina Battistini, Andrea Ascoli Marchetti, Arnaldo Ippoliti
Vascular Surgery Unit, Department of Biomedicine and Prevention, University of Rome Tor Vergata, Rome, Italy
Abstract
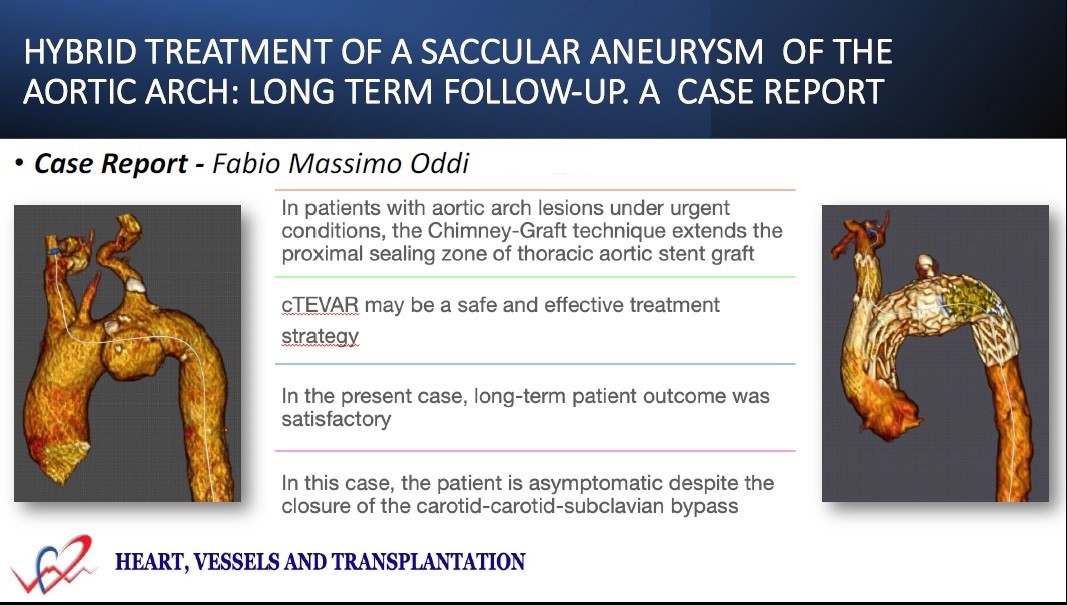
Objective: We describe a complex urgent clinical case of aortic arch aneurysm treated with a hybrid intervention with a medium-long follow-up.
Case presentation: A 67-years-old man presented to the emergency room for chest pain. The computed tomography angiography (CTA) documented the presence of saccular aneurysm of the aortic arch. First stage of the hybrid intervention was performed as carotid-carotid-subclavian-bypass using 7-mm PTFE graft with ringed support. The saccular aneurysm was repaired by placing a thoracic endovascular stent graft (Gore C-TAG) with Chimney technique (cTEVAR) in the anonymous trunk (with Gore Excluder Iliac Extension) to create a suitable proximal landing zone in Zone 0. Then the procedure was completed with occlusion of the left subclavian artery by plug. Final angiography and post-operative CTA document the absence of endoleaks, patency of the Chimney and bypass. At the 4th year of follow-up with Doppler ultrsound and CTA, we unexpectedly found carotid-subclavian bypass occlusion. The patient is completely asymptomatic and apparently in excellent condition at the 8-years follow-up. The Chimney is still pervious, the prosthesis is correctly placed, and the lesion has gone through complete shrinkage.
Conclusion: The hybrid treatment combined with Chimney of the arch in urgent setting provides good outcomes in the medium to long term as in this case. In the present case, mid-term patient outcome was satisfactory and the patient is asymptomatic despite the closure of the bypass.
Key words: Aneurysm, aortic arch, hybrid repair, TEVAR, Chimney technique
Introduction
Thoracic aortic disease affecting the arch and proximal descending thoracic aorta is still a challenge (1). Open surgery for aortic arch disease carries a high risk of significant morbidity and mortality. Therefore, many patients with severe comorbidities or unfavorable anatomy are less suitable for open surgical repair (2).
Good results for endovascular repair require careful patient selection and high-volume activity but remain a challenge in elderly patients and emergency scenarios. The aortic arch presents specific challenges because of the acute angle of the arch, its branches, high blood flow, and the pulsatile nature of the proximal aorta (3).
Hybrid procedures (endovascular repair combined with conventional open surgery - HAAR) to treat extensive aortic disease may be an alternative treatment and for some high-risk patients (1, 4). Several studies describe great results, but with short follow up.
In this regard, we describe a case of a saccular aneurysm of the aortic arch treated with a hybrid surgery and with a follow up of 8 years.
Case report
We report the case of a 67-year-old man, obese with a history of hypertension, chronic obstructive pulmonary disease, and Kaposi sarcoma, was admitted to the emergency room for chest and retroscapular pain that had arisen about 5 days earlier. He had previous pulmonary embolism and he subjected to endovascular exclusion of the aneurysm (EVAR) for aortic arch aneurysm (AAA) three years earlier.
Thus, he underwent a computed tomography angiography (CTA), which detected sacciform aneurysm of the aortic arch on the anterocaudal side in the portion between the carotid artery and the left subclavian artery (Fig. 1).

Figure 1. Computed tomography angiography view of saccular aneurysm of the aortic arch on the anterocaudal side in the portion between the carotid artery and the left subclavian artery
It was decided to proceed urgently with a hybrid surgical treatment consisting of carotid-carotid-subclavian bypass, after that we proceeded with an EVAR with a Chimney on the anonymous trunk and a thoracic endovascular aortic repair (TEVAR), and finally completed the treatment with the occlusion of the left subclavian artery with a plug.
The patient firstly underwent a carotid-carotid-subclavian bypass (CCSB) with an armed polytetrafluoroethylene (PTFE) prosthesis.
After induction of general anesthesia with the patient in the supine position, a longitudinal incision was created on the right neck with routine dissection of the right common carotid artery.
A longitudinal left supraclavicular incision was created to access the subclavian and carotid arteries. The left subclavian artery and left common carotid arteries were mobilized and a 7-mm PTFE graft with ringed support was positioned (Fig. 2).

Figure 2. Carotid-carotid-subclavian bypass
A detailed planning showed us that the length to be covered taking into account the chimney on the trunk was between 15 and 17 cm. The proximal landing is 35 mm in diameter while the distal is 26 mm. The brachiocephalic trunk had a diameter of 15 cm at the origin and of 12 cm distally. (Fig. 3) We opted for the use of a Gore Ctag. The partial deployment, the active control, the low radial force, and the high conformability make it a suitable prosthesis not only in the aortic arch pathologies, but also in chimneys. We therefore opted for a 34-100 distally and for a 45-100 proximally to achieve precisely a 30% oversizing in the sealing zones. For the brachiocephalic trunk, we opted for two legs, normally used in internal iliac artery.
The procedure was totally percutaneous, after the placement of cardiac pacing. We released the distal module; we placed the two internal iliac components and finally we proceeded with the placement and replacement of the proximal module by partial deployment and angulation control. After, we embolized the left subclavian artery with a plug. The conclusive angiography evidenced the absence of endoleaks, the patency of the Chimney and the bypass. Prior to the discharge, a CT check performed on the patient documented the patency of the vertebral and carotid arteries and the bypass, some artifacts due to the motion and the correct positioning of prosthetic modules in the absence of endoleaks (Fig. 4). The patient was discharged on the 5th post-operative day with dual antiplatelet therapy.
A previous CT (performed 2 years ago) showed that the arch lesion was already/clearly visible and that this has grown in size over time. You can notice an increase of the diameter of the lesion emphasizing the progression of aortic pathology. At the 4th year after procedure, on ultrasounds follow-up we unexpectedly found the occlusion of the carotid-subclavian bypass (Fig. 5). The patient was completely asymptomatic and apparently in excellent condition.
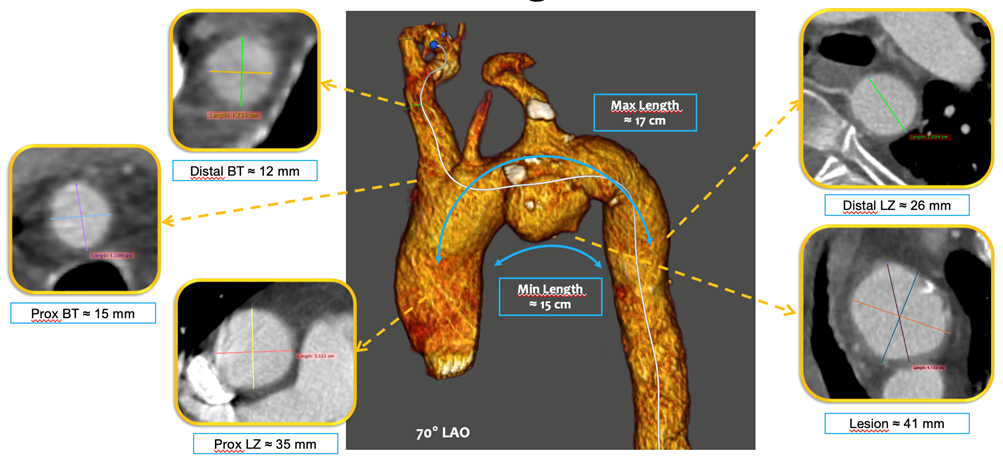
Figure 3. This planning shows that the length to be covered taking into account the Chimney on the trunk was between 15 and 17 cm. The proximal landing is 35 mm in diameter while the distal is 26 mm. The anonymous trunk had a diameter of 15 cm at the origin and of 12 cm distally.
BT - brachiocephalic trunk, LZ – landing zone

Figure 4. Computed tomography ngiography after procedure documented the patency of the Chimney graft and the absence of endoleaks
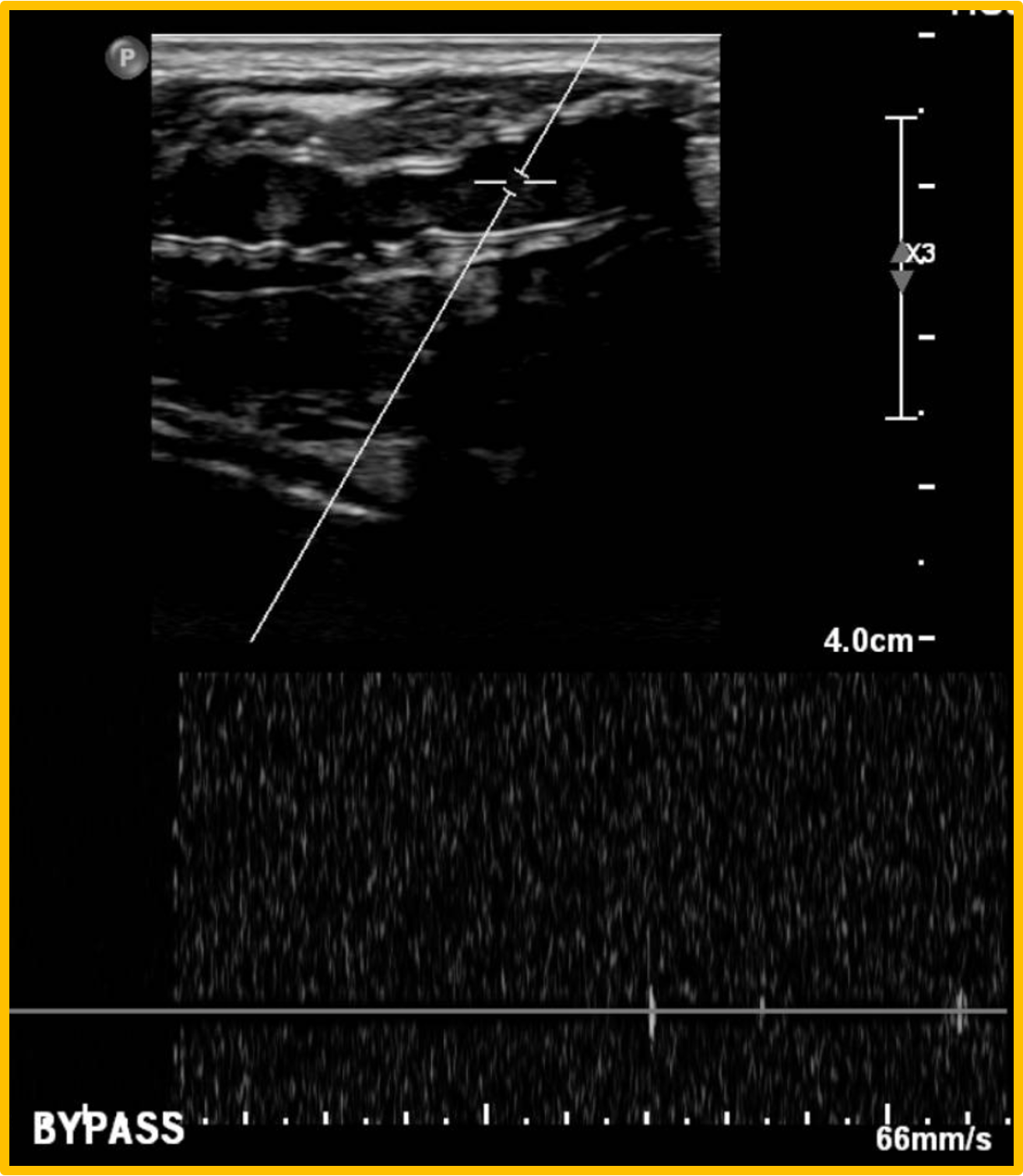
Figure 5. The Doppler ultrasound documented the occlusion of the carotid-subclavian bypass
The CT scan was prescribed, and it confirmed the previous diagnosis; the Chimney was still previous, the prosthesis was correctly positioned, and the lesion has gone through a complete shrinkage. The patient is completely asymptomatic and apparently in excellent condition at the 8-years follow-up.
Discussion
Aortic syndromes, ranging from acute dissections to chronic aneurysms, present unique complexities, where timely and accurate diagnosis can profoundly impact patient outcomes (5).
HAAR consists of thoracic stent-graft repair and procedures to maintain cerebral blood flow. Several hybrid techniques have been used, including arch artery debranching, parallel graft technique, fenestration or branching of endograft, or a combination of these (6).
The 30-day mortality was similar between the total AAA and hybrid patients (3% vs. 2%, p=0.76), though the hybrid arch patients had significantly shorter intensive care unit (p<0.001) and hospital (p=0.015) lengths of stay (7). Our strategy was a hybrid treatment, which as documented by several studies in the literature, provided good results in arch pathology (8-11). When choosing treatment, several aspects must be considered: primarily the anatomy of the aortic arch variations, the etiology of the disease, the diseased areas and the patient's comorbidities. When dealing with complex aortic pathologies, the first choice should be hybrid treatment in suitable patients due to its less invasive nature (12).
While hybrid treatments offer promising short-term outcomes, questions remain regarding their long-term durability and effectiveness, particularly in younger patients with a longer life expectancy (13). In the case described, the follow-up is 8 years, the patient is in good general condition, and the prosthesis is correctly positioned in the absence of endoleak or other complications, with complete shrinkage of the residual sac.
The clinical presentation of CCSB occlusion may vary depending on the extent and rapidity of bypass occlusion. Patients may present with symptoms of cerebral ischemia. The management of CCSB occlusion requires a multidisciplinary approach and should be tailored to the individual patient's clinical presentation, comorbidities, and anatomical considerations. Conservative measures, including antiplatelet therapy and risk factor modification, may be appropriate for asymptomatic patients or those with minimal symptoms (14).
In the case reported, the bypass probably did not occlude quickly and the patient was completely asymptomatic. For this reason, he was not subjected to a recanalization attempt. Hybrid surgical interventions appear to possess all positive properties of endovascular and traditional open surgery, thus allowing of both avoiding threatening complications and minimizing the terms of rehabilitation. This technique might thus be considered a useful tool to be included into the basic armamentarium of the vascular surgeon as an option of revascularization (15).
Conclusion
The hybrid treatment combined with Chimney of the arch allows extending the sealing zone and provides good outcomes in the medium to long term as in this case. In patients with aortic arch lesions under urgent conditions, the Chimney technique extends the proximal sealing zone of thoracic aortic stent graft and the cTEVAR may be a safe and effective treatment strategy. In the present case, mid-term patient outcome was satisfactory and the patient is asymptomatic despite the closure of the bypass. Further research is needed with large comparative studies to consolidate the results of this hybrid treatment and define its role in the management of aortic arch disease.
Ethics: Patient`s informed consent was obtained for all procedures
Peer-review: External and Internal
Conflict of interest: None to declare
Authorship: F.M.O., G.G., M.F., M.B., A.A.M., and A.I. equally participated in case management and preparation of manuscript, thus fulfilled authorship criteria.
Acknowledgement and funding: None to declare
Statement on A.I.-assisted technologies use: Authors reported they did not use A.I.- assisted technologies in preparation of manuscript
References
| 1.Ferrero E, Ferri M, Viazzo A, Robaldo A, Zingarelli E, Sansone F, et al. Is total debranching a safe procedure for extensive aortic-arch disease? A single experience of 27 cases. Eur J Cardiothorac Surg 2012; 41: 177-82. https://doi.org/10.1016/j.ejcts.2011.05.058 |
||||
| 2.Lu H, Huang LC, Chen LW. Endovascular surgery for thoracic aortic pathologies involving the aortic arch. Front Cardiovasc Med 2022; 9: 927592. https://doi.org/10.3389/fcvm.2022.927592 |
||||
| 3.Lioupis C, Abraham CZ. Results and challenges for the endovascular repair of aortic arch aneurysms. Perspect Vasc Surg Endovasc Ther 2011; 23: 202-13. https://doi.org/10.1177/1531003511413608 |
||||
| 4.Elhelali A, Hynes N, Devane D, Sultan S, Kavanagh EP, Morris L, et al. Hybrid repair versus conventional open repair for thoracic aortic arch aneurysms. Cochrane Database Syst Rev 2021; 6: CD012923. https://doi.org/10.1002/14651858.CD012923.pub2 |
||||
| 5. Oddi FM, Granata G, Oddi L, Fedeli G, Brizzi V. The 24th organ: the aorta. The main concept of new EACTS/STS Guidelines. Heart Vessels Transplant 2024; 8: doi: 10.24969/hvt.2024.481 https://doi.org/10.24969/hvt.2024.481 |
||||
| 6- Morishita K. Hybrid aortic arch repairs. Ann Vasc Dis 2019; 12: 14-20. https://doi.org/10.3400/avd.ra.19-00008 |
||||
| 7. Xydas S, Mihos CG, Williams RF, LaPietra A, Mawad M, Wittels SH, et al. Hybrid repair of aortic arch aneurysms: a comprehensive review. J Thorac Dis 2017; 9: S629-34. https://doi.org/10.21037/jtd.2017.06.47 |
||||
| 8- Kieffer E, Bahnini A, Koskas F. Aberrant subclavian artery: surgical treatment in thirty-three adult patients. J Vasc Surg 1994; 19: 100-11. doi: 10.1016/S0741-5214(94)70125-3 https://doi.org/10.1016/S0741-5214(94)70125-3 |
||||
| 9.Oddi FM, Franceschini G, Oddi L, Fedeli G. 2022 American Heart Association/American College of Cardiology guidelines for the diagnosis and management of aortic disease: lessons to be drawn. Heart Vessels Transplant 2023; 7: 14-6. doi: 10.24969/hvt.2023.374 https://doi.org/10.24969/hvt.2023.374 |
||||
| 10. Yang C, Shu C, Li M, Li Q, Kopp R. Aberrant subclavian artery pathologies and Kommerell's diverticulum: a review and analysis of published endovascular/hybrid treatment options. J Endovasc Ther 2012; 19: 373-82. doi: 10.1583/11-3673MR.1 https://doi.org/10.1583/11-3673MR.1 |
||||
| 11. Jalaie H, Grommes J, Sailer A, Greiner A, Binnebösel M, Kalder J, et al. Treatment of symptomatic aberrant subclavian arteries. Eur J Vasc Endovasc Surg 2014; 48: 521-6. doi: 10.1016/j.ejvs.2014.06.040 https://doi.org/10.1016/j.ejvs.2014.06.040 |
||||
| 12. Akbulut M, Ak A, Ozturker K, Sismanoglu M, Tuncer MA. Hybrid treatment of complex aortic arch anomaly with saccular aneurysm. Braz J Cardiovasc Surg 2019; 34: 769-71. https://doi.org/10.21470/1678-9741-2018-0229 |
||||
| 13. Vekstein AM, Jensen CW, Weissler EH, Downey PS, Kang L, Gaca JG, et al. Long-term outcomes for hybrid aortic arch repair. J Vasc Surg 2024;79: 711-720.e2. doi: 10.1016/j.jvs.2023.11.032 | ||||
| 14.Kuo WT, Gould MK, Louie JD, Rosenberg JK, Sze DY, Hofmann LV. Catheter-directed therapy for the treatment of massive pulmonary embolism: systematic review and meta-analysis of modern techniques. J Vasc Interv Radiol 2009; 20: 1431-40. https://doi.org/10.1016/j.jvir.2009.08.002 |
||||
| 15. Akchurin RS, Imaev TE, Komlev AE, Osmanov MR, Nikonova ME, Pokidkin IA. Hybrid surgical management of a saccular aneurysm of the aortic arch. Angiol Sosud Khir 2011; 17: 142-6. | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

