Severe, rapidly evolving infective endocarditis as a complication of elective surgery: a case report
CASE REPORT
Severe, rapidly evolving infective endocarditis as a complication of elective surgery: a case report
Article Summary
- DOI: 10.24969/hvt.2024.521
- CARDIOVASCULAR DISEASES
- Published: 15/10/2024
- Received: 05/09/2024
- Revised: 02/10/2024
- Accepted: 03/10/2024
- Views: 4091
- Downloads: 2587
- Keywords: Infective endocarditis, Staphylococcus aureus; complications, elective surgery, case report
Address for Correspondence: Ezequias Batista Martins, Rua Des. Athayde Parreiras, 100, Fátima, Niterói, Rio de Janeiro, 24070-090, Brazil
Email: ezequiasm@id.uff.br Phone: +55 (21) 2629-9303
ORCID: Roxana Flores Mamani - 0000-0003-0794-8366; Ezequias Batista Martins -0000-0003-3373-0408; Paulo Afonso Daflon Mendonca - 0009-0007-1616-8720; Rivelino Trindade de Azevedo - 0000-0003-1819-0204; Diego Amorim Fraca-0000-0001-8266-3905; Julian Camilo Alfonso Diaz - 0009-0001-8464-9848; Nathalia da Fonte Konig - 0009-0006-5821-0045; Cristina da Cruz Lamas -0000-0002-5561-999X
Roxana F. Mamani1,2, Ezequias B. Martins2,3*, Paulo A.D. Mendonca1, Rivelino T. Azevedo1, Diego A. Fraca1, Julian C.A. Diaz1, Nathalia F. Konig1, Victor C.M. Fernandes1, and Cristiane C. Lamas2,4
1Ronaldo Gazolla Municipal Hospital, Rio deJaneiro, Rio de Janeiro, Brazil
2Evandro Chagas National Institute of Infectious Diseases, Fiocruz, Rio de Janeiro, Brazil
3Faculty of Medicine, Federal Fluminense University, Niteroi, Rio de Janeiro, Brazil
4National Institute of Cardiology, Rio de Janeiro, Brazil
Abstract
Objective: Staphylococcus aureus infective endocarditis is a serious disease and often affects previously healthy or minimally calcified heart valves in the hospital setting. We report a case of rapidly evolving Staphylococcus aureus endocarditis in a 64-year-old diabetic man with minimally calcified aortic and mitral valves, in the postoperative period of elective abdominal surgery.
Сase Presentation: A 64-year-old diabetic, morbidly obese and hypertensive man was admitted on May 14, 2024 to undergo an umbilical herniorrhaphy. He suffered from a rapidly evolving Staphylococcus aureus endocarditis in the postoperative period of elective abdominal surgery. S.aureus bacteremia was related to temporary intravenous lines, which were removed. The patient evolved with hypotension and confusion, requiring intensive care. He died 2 weeks later of ventilator- associated pneumonia.
Conclusion: Intravenous lines may be the source of bacteremia and sepsis, S. aureus is one of the most common agents, and may seed heart valves, with high rates of morbidity and mortality. Transthoracic and transesophageal echocardiograms are crucial to establish endocarditis diagnosis.
Key words: Infective endocarditis, Staphylococcus aureus; complications, elective surgery, case report
Introduction
Worldwide, virulent staphylococci represent one of the main causative agents of infective endocarditis (IE), and fighting this infection represents one of the main challenges in public health services (1).The diagnosis of IE is based on major criteria patterns (bacteremia and images showing endocardial changes) and minor criteria (2). Staphylococcus aureus bacteremia and specially endocarditis is associated with a high mortality (3). The diagnosis of IE entails prolonged administration of antibiotics and rapid assessment for the need for heart valve surgery (4).
If Staphylococcus aureus bacteremia is confirmed, the risk of IE is variable and dependent on factors related to both bacteremia and the patient (5). The main risk factors related to the patient are: previous heart disease, illicit intravenous drug use, heart valve surgery and use of cardiac implanted electronic devices (6-8). The main factors related to bacteremia refer to the bacterial load, expressed as blood culture shorter times to positivity and persistent bacteremia (9).
Graphical abstract
We report a serious case of rapidly evolving S. aureus endocarditis in a 64-year-old diabetic man without previous heart disease, in the postoperative period of elective abdominal surgery.
Case Report
A 64-year-old diabetic, morbidly obese and hypertensive man was admitted on May 14, 2024 to undergo an umbilical herniorrhaphy. During the first seven days after surgery, the surgical wound became infected and there was dehiscence of the surgical stitches. Upon readmission, a tumor mass was identified through an abdominal computed tomography (CT) examination; it was located in the ascending colon, close to the hepatic angle.
Fourteen days later (May 28, 2024), a new umbilical herniorrhaphy was performed and part of the ascending colon was removed to extract the tumor. Treatment with Ciprofloxacin (800 mg/day) and Metronidazole (1,500 mg/day) was carried out for ten days. On the 11th postoperative day (June 08, 2024) of the second surgery, he developed hypotension, tachycardia and diarrhea. On the same day, the intravenous lines were removed, and blood cultures were collected.
Three days later (June 11, 2024), the patient became unconscious, disoriented. On physical examination her mucous membranes were dehydrated, hypochloric, anicteric; she had tachycardia, tachypnea, hypotension, rhythmic heartbeats of preserved intensity, preserved vesicular murmur in both hemithoraxes; there were no lesions on mucous membranes and skin. She was hydrated with aliquots without response. He was transferred to the intensive care unit (ICU) and underwent orotracheal intubation, sedation and administration of inotropes. Empirical treatment with vancomycin (2.000 mg/day) and piperacillin/tazobactam (18.000 mg/day) was started. Blood cultures (4 samples out of 4) grew methicillin-resistant S. aureus. Piperacillin/tazobactam was stopped and vancomycin was maintained, at the same initial dose.
The laboratory tests performed during ICU admission indicated features suggestive of serious bacterial infection, mainly leukocytosis, thrombocytopenia and elevated C-reactive protein values (Table 1).
A transesophageal echocardiogram (TEE) performed 2 days after ICU admission (June 13, 2024) showed destruction (rupture) of the anterior leaflet of the mitral valve, mild mitral and aortic regurgitation, corroborating the diagnosis of IE (Fig. 1). Other findings include estimated pulmonary artery systolic pressure (PASP) of 26 mmHg and an ejection fraction of 65%. A previous transthoracic echocardiography done 3 weeks earlier showed minimally calcified aortic and mitral valves, compatible with his age.
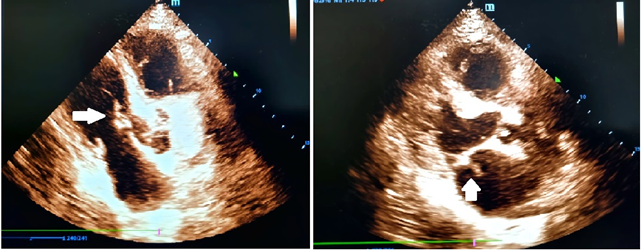
Figure 1. Transthoracic echocardiogram showed destruction (rupture) of the anterior leaflet of the mitral valve and presence of a vegetative lesion (arrows)
After 7 days of culture-guided treatment (vancomycin), pan-resistant Providencia rettgeri was identified in 4/4 blood samples, and the patient developed clinical and hemodynamic worsening. On the 11th day of vancomycin, polymyxin B were administered empirically, and the patient was recultured, isolating Pseudomonas aeruginosa (4/4 blood culture bottles) sensitive to polymyxin B and ceftazidime-avibactam (Table 2).
After seven days in the ICU (June 18, 2024), the infection progressively worsened, with fever and hemodynamic instability persisting. Chest CT showed septic pulmonary embolization and brain CT showed a hypodense image compatible with subacute ischemia, secondary to embolism. Polymyxin B (3 million/day) was added to treat ventilator-associated pneumonia. Hemodialysis sessions were necessary. Fifteen days after hospital admission (June 25, 2024), the patient developed multiple organ failure and died (on the 15th day in the ICU).
Discussion
This case report showed a rapidly evolving IE in a patient without previous heart disease, demonstrating the great potential for morbidity and mortality of S. aureus.
Staphylococcus aureus produces conditions range from uncomplicated bacteremia to fulminant infective endocarditis (9).
|
Table 1. Laboratory tests performed during hospitalization (2024) |
|||||||||||
|
|
May 27 |
Jun 02 |
Jun 08 |
Jun 11 |
Jun 13 |
Jun 15 |
Jun 17 |
Jun 20 |
Jun 23 |
Jun 24 |
Jun 25 |
|
Hemoglobin, g/dL |
9.8 |
10.5 |
8.9 |
8.6 |
8.6 |
7.7 |
7.4 |
7.6 |
7.3 |
8.5 |
9.4 |
|
Hematocrit , % |
29.4 |
31.5 |
26.7 |
25.8 |
24.7 |
23.1 |
21.8 |
22.8 |
21.9 |
24.1 |
28.2 |
|
White blood cells, x103/µL |
5.250 |
7.410 |
8.890 |
16.560 |
18.840 |
23.050 |
26.590 |
31.480 |
25.580 |
21.550 |
27.410 |
|
Bands cells, % |
2 |
2 |
2 |
4 |
3 |
6 |
5 |
8 |
6 |
6 |
7 |
|
Platelets, x103/µL |
153.000 |
116.000 |
115.000 |
68.000 |
70.000 |
115.000 |
170.000 |
271.000 |
259.000 |
207.000 |
204.000 |
|
Alanineaminotransferase , IU/L |
19 |
--- |
--- |
28 |
--- |
--- |
--- |
34 |
--- |
--- |
--- |
|
Alkaline phosphatase, IU/L |
10 |
--- |
--- |
27 |
--- |
--- |
--- |
10 |
--- |
--- |
--- |
|
International normalized ratio |
1.11 |
--- |
--- |
1.37 |
1.30 |
1.20 |
1.10 |
--- |
--- |
--- |
--- |
|
Blood urea nitrogen, mg/dL |
15 |
20 |
44 |
60 |
65 |
85 |
176 |
215 |
86 |
31 |
46 |
|
Creatinine, mg/dL |
0.9 |
0.84 |
1.08 |
1.35 |
1.60 |
2.10 |
4.20 |
3.84 |
1.97 |
1.00 |
1.65 |
|
Potassium, mEq/L |
4.0 |
4.0 |
3.1 |
3.4 |
4.0 |
4.9 |
4.5 |
5.0 |
3.6 |
4.0 |
3.5 |
|
C-reactive protein, mg/dL |
9.4 |
1.74 |
3.14 |
15.0 |
14.3 |
13.6 |
12.2 |
16.4 |
16.2 |
14.0 |
17.1 |
|
Glucose, mmol/L |
100 |
110 |
70 |
146 |
195 |
275 |
169 |
209 |
100 |
130 |
60 |
|
Table 2. Cultures performed during hospitalization |
|||
|
Date |
Microorganism |
Antibiogram |
|
|
Sensitive |
Resistant |
||
|
June 8, 2024 |
Staphylococcus aureus (MRSA, blood culture)
|
Vancomycin/Daptomycin/Linezolid/Teicoplamin/ Tigecycline/Co-trimoxazole |
Oxacillin / Ciprofloxacin / Clindamycin Erythromycin / Levofloxacin/Gentamicin |
|
June 11, 2024 |
Staphylococcus aureus (MRSA, blood culture) |
Vancomycin/Daptomycin/Gentamicin Linezolid/Teicoplamin/Tigecycline/co-trimoxazole |
Oxacillin / Ciprofloxacin / Clindamycin Erythromycin / Levofloxacin |
|
June 17, 2024 |
Providencia rettgeri (blood culture) |
None |
Amikacin / Ampicillin-Sulbactam / CefepimeCeftazidime / Ceftriaxone / Cirpofloxacin Ertapenem/Gentamicin/Imipenem Levofloxacin/Meropenem/Piperacillin-Tazobactam Polymycin B |
|
June 20, 2024 |
Pseudomonas aeroginosa (blood culture) |
Ceftazidime-Avibactam Polymycin B |
Amikacin / Cefepime / Ceftazidime / Ciprofloxacin Gentamicin / Imipenem / Levofloxacin / Meropenem Piperacillin-Tazobactam |
|
June 20, 2024 |
Acinetobacter baumannii (tracheal secretion) |
Polymycin B |
Amikacin / Ciprofloxacin / Gentamicin Imipenem / Levofloxacin / Meropenem / Tigecycline |
Approximately 25% of patients with S. aureus bacteremia develop IE (9), with an in-hospital mortality rate ranging between 25% and 46% (10). About 40% of individuals with IE due to S. aureus have no known risk factors (9). The diagnosis of IE in our patient was relatively quick, being confirmed by TEE 2 days after confirmation of S. aureus bacteremia.
S. aureus interacts with the host's innate immunity, interfering with protection mechanisms through two coagulases (the von Willebrand factor binding protein and coagulase), producing a fibrinogen/fibrin complex that stimulates the formation of large vegetations, causing symptomatic embolic events (11). The patient presented in this report was diabetic and elderly, factors that corroborate a less efficient immunological response.
The diagnosis of IE is based on the 2023 Duke-ESC and Duke-ISCVID Clinical Criteria, showing greater sensitivity (82% and 81%, respectively) compared to the 2015 Duke-ESC (75%) for S. aureus IE (12), according to the analysis of physical examination, echocardiography, microbiological examinations and imaging findings of target organs (13). Early diagnosis leads to appropriate antibiotic treatment and, when indicated, surgical intervention, resulting in reduced morbidity and mortality (13). Current guidelines recommend routine transthoracic echocardiography (TTE) for patients with S. aureus bacteremia; TEE is reserved for cases where the initial TTE is normal and clinical suspicion of IE remains high (9 ,12, 14). In our case report, diagnostic procedures were carried out in a timely manner and appropriate antibacterial treatment was instituted, but the infection progressed rapidly, resulting in a fatal outcome. Furthermore, gram-negative superinfections occurred, related to mechanical ventilation, which further compromised the patient’s general status.
A systematic review from 2022, with a total of 2 222 patients with a confirmed diagnosis of IE, observed an increased prevalence for some comorbidities, such as cardiovascular disease, diabetes mellitus and cancer. Mortality was higher in adults over 65 years of age, mainly because they were unable to undergo surgery, due to the increased risk of post-surgical complications (15).The patient in this case presented some associated risk factors, such as diabetes mellitus, prolonged hospitalization and use of an intravascular catheter, and he was 64 years old.
Bloodstream infections related to central venous catheters are common in ICUs. In contrast to other nosocomial infections, most of the risk factors for this infection are related to the intravascular device and can be prevented (16), being considered a common iatrogenic condition with an estimated incidence of 4.1 per 1,000 days (17). Bell et al. (18), in 2016, carried out a study with 254 patients with bloodstream infections, of which 45 isolated S. aureus, 35 (13.8%) developed at least one hematogenous complication (14%), including suppurative thrombophlebitis (n = 15), endocarditis (n = 7) and metastatic infections (n = 16). Infections caused by S. aureus have been associated with an increased risk of hematogenous complications. Diabetes mellitus, maintenance of deep venous access and hematogenous complications were associated with increased 3-month mortality (18).
The primary complications of IE include valve regurgitation, heart failure, embolic events, and sepsis (12, 14). The three main indications for surgery in patients with native valve IE are: heart failure due to valve dysfunction or perforation, uncontrolled endocardial infection (e.g., paravalvular extension or persistent bacteremia), and prevention of systemic embolization, especially to the brain (13). In the case reported, the patient presented with pulmonary and cerebral embolization, factors that contributed to death. Due to the rapid evolution of the case, surgery was not considered.
In a prospective cohort study (19) carried out from 2000 to 2005, with 2781 adult patients with IE, S. aureus was the most common pathogen (31.2%), and mitral and aortic valves (41.1% and 37.6 %, respectively) were the most frequently infected. The most common complications were: stroke (16.9%), embolization other than stroke (22.6%), heart failure (32.3%) and intracardiac abscess (14.4%). S. aureus infection, mitral valve vegetation, and paravalvular complications were associated with an increased risk of in-hospital death (19). Based on the previous studies mentioned, we confirmed that this was a classic case, with mitral valve involvement, cerebral emboli and septic shock.
Conclusion
S. aureus bacteremia was associated with intravenous line infection in a diabetic obese man, and seeded heart valves and the lungs. Infective endocarditis was quickly diagnosed, and antibiogram-guided treatment was instituted, demonstrating the expertise of the medical team. However, the aggressive destructive potential of S. aureus was decisive for the rapid deterioration of the heart valve function, and the need for mechanical ventilation resulted in further infections.
Important take home messages are: i) beware of intravenous line infections; ii) once S.aureus bacteremia is documented, it is crucial to investigate infective endocarditis even in patients with minimally calcified valves.
Ethics: Informed consent was obtained from all the subjects involved in
the study. The local ethics committee reviewed and approved the study and assigned the approval number: CAAE: 81696324.2.0000.5262.
Peer-review: External and Internal
Conflict of interest: None to declare
Authorship: R.F.M, E.B.M., P.A.D.M, R.T.A., D.A.F., J.C.A.D., N.F.K., and V.C.M.F. equally contributed to case management and preparation of manuscript for publication. C.C.L. managed and reviewed the manuscript. All authors reviewed final version and fulfilled authorship criteria.
Acknowledgement: The authors would like to thank the patient's family for authorizing participation in this study and all the employees at Hospital Municipal Ronaldo Gazolla, Brazil
Funding: None to declare
Statement on A.I.-assisted technologies use: Authors declared they did not use A.I.- assisted technologies in preparation of manuscript
References
| 1.Nappi F, Avtaar Singh SS. Host-bacterium interaction mechanisms in Staphylococcus aureus endocarditis: A systematic review. Int J Mol Sci 2023; 24: 11068. https://doi.org/10.3390/ijms241311068 |
||||
| 2. Fowler VG, Durack DT, Selton-Suty C, Athan E, Bayer AS, Chamis AL, et al. The 2023 Duke-international society for cardiovascular infectious diseases criteria for infective endocarditis: updating the modified Duke criteria. Clin Infect Dis 2023; 77: 518e26. https://doi.org/10.1093/cid/ciad271 |
||||
| 3.Bai AD, Lo CKL, Komorowski AS, Suresh M, Guo K, Garg A, et al. Staphylococcus aureus bacteraemia mortality: a systematic review and meta-analysis. Clin Microbiol Infect 2022; 28: 1076e84 https://doi.org/10.1016/j.cmi.2022.03.015 |
||||
| 4.Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European society of cardiology (ESC). Endorsed by: European association for cardio-thoracic surgery (EACTS), the European association of nuclear medicine (EANM). Eur Heart J 2015; 36: 3075e128. https://doi.org/10.1093/eurheartj/ehv319 |
||||
| 5.Rasmussen M, Gilje P, Fagman E, Berge A. Bacteraemia with gram-positive bacteria-when and how do I need to look for endocarditis? Clin Microbiol Infect 2024; 30: 306-11. https://doi.org/10.1016/j.cmi.2023.08.027 |
||||
| 6.Sousa C, Botelho C, Rodrigues D, Azeredo J, Oliveira R. Infective endocarditis in intravenous drug abusers: an update. Eur J Clin Microbiol Infect Dis 2012; 31: 2905e10. https://doi.org/10.1007/s10096-012-1675-x |
||||
| 7. Ostergaard L, Valeur N, Wang A, Bundgaard H, Aslam M, Gislason G, et al. Incidence of infective endocarditis in patients considered at moderate risk. Eur Heart J 2019; 40: 1355e61. https://doi.org/10.1093/eurheartj/ehy629 |
||||
| 8. Ostergaard L, Valeur N, Ihlemann N, Bundgaard H, Gislason G, Torp Pedersen C, et al. Incidence of infective endocarditis among patients considered at high risk. Eur Heart J 2018; 39: 623e9. https://doi.org/10.1093/eurheartj/ehx682 |
||||
| 9. van der Vaart TW, Prins JM, Soetekouw R, van Twillert G, Veenstra J, Herpers BL, et al. prediction rules for ruling out endocarditis in patients with staphylococcus aureus bacteremia. Clin Infect Dis Off Publ Infect Dis Soc Am 2021; 74: 1442-9. https://doi.org/10.1093/cid/ciab632 |
||||
| 10.Khan UA, Zaidi SH, Majeed H, Lopez E, Tofighi D, Andre P, et al. Clinical risk factors for infective endocarditis patients with staphylococcus aureus bacteremia and the diagnostic utility of transesophageal echocardiogram. Curr Probl Cardiol 2022; 47: 101331. https://doi.org/10.1016/j.cpcardiol.2022.101331 |
||||
| 11.Chambers HF, Bayer AS. Native-Valve Infective Endocarditis. N Engl J Med 2020; 383: 567-76. https://doi.org/10.1056/NEJMcp2000400 |
||||
| 12.Delgado V, Ajmone Marsan N, de Waha S, Bonaros N, Brida M, Burri H, et al. 2023 ESC Guidelines for the management of endocarditis. Eur Heart J 2023; 44: 3948-4042. https://doi.org/10.1093/eurheartj/ehad193 |
||||
| 13.Budea CM, Bratosin F, Bogdan I, Bota AV, Turaiche M, Tirnea L, et al. Clinical presentation and risk factors of infective endocarditis in the elderly: A systematic review. J Pers Med 2023; 13: 296. https://doi.org/10.3390/jpm13020296 |
||||
| 14.Buetti N, Timsit JF. Management and prevention of central venous catheter-related infections in the ICU. Semin Respir Crit Care Med 2019; 40: 508-23. https://doi.org/10.1055/s-0039-1693705 |
||||
| 15.Rosenthal VD, Al-Abdely HM, El-Kholy AA, AlKhawaja SAA, Leblebicioglu H, Mehta Y, et al. International nosocomial infection control consortium report, data summary of 50 countries for 2010-2015: Device-associated module. Am J Infect Control 2016; 44: 1495-504. https://doi.org/10.1016/j.ajic.2016.08.007 |
||||
| 16.Bell EC, Chapon V, Bessede E, Meriglier E, Issa N, Domblides C, et al. Central venous catheter-related bloodstream infections: Epidemiology and risk factors for hematogenous complications. Infect Dis Now 2024 ;54: 104859. https://doi.org/10.1016/j.idnow.2024.104859 |
||||
| 17.Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG, Bayer AS, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009; 169: 463-73. https://doi.org/10.1001/archinternmed.2008.603 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

