Angiogenesis monitoring after organ transplantation – Should we address it?
EDITORIALS
Angiogenesis monitoring after organ transplantation – Should we address it?
Article Summary
- DOI: 10.24969/hvt.2024.541
- CARDIOVASCULAR DISEASES
- Published: 19/01/2025
- Received: 16/01/2025
- Accepted: 17/01/2025
- Views: 3081
- Downloads: 2280
- Keywords: angiogenesis, transplantation, monitoring
Address for Correspondence: Vitaliy Petrov, Department of Surgery and Transplantology, Danylo Halytsky National Medical University, Lviv, Ukraine
E-mail: vtly.12@gmail.com ORCID: 0000-0002-2205-5403
Vitaliy Petrov, Department of Surgery and Transplantology, Danylo Halytsky National Medical University, Lviv, Ukraine
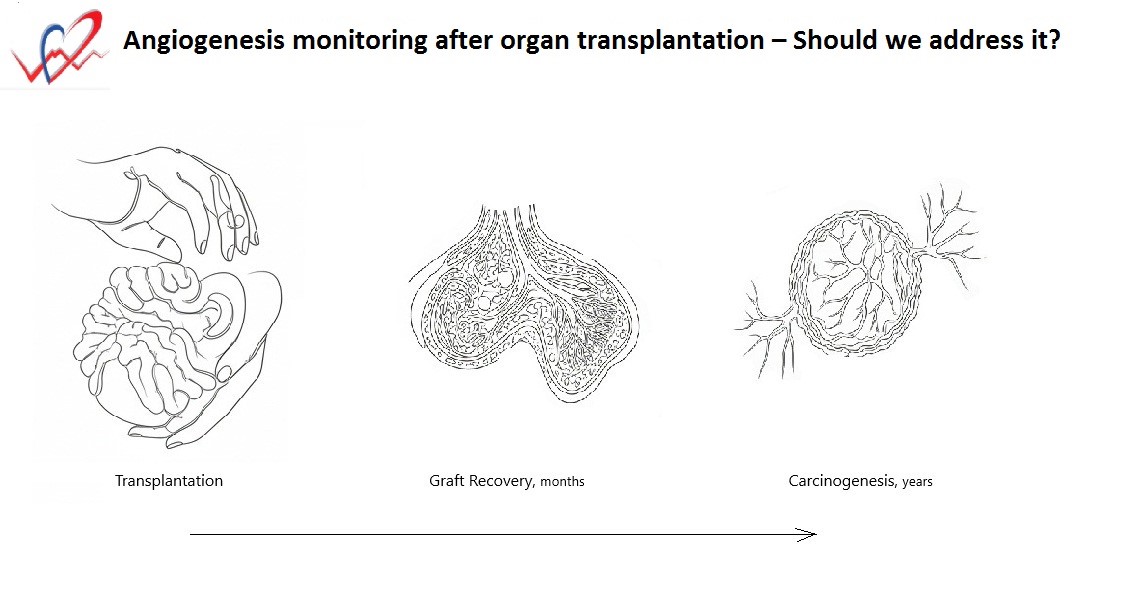
Graphical abstract
Key words: angiogenesis, transplantation, monitoring
![]()
Organ transplantation offers unique opportunities to patients with advanced organ diseases. These opportunities include the significantly improved survival and quality of life. Two examples may be given to demonstrate the gains.
The first scenario is heart failure. The expected life span of an individual with advanced heart failure may be as short as twelve to twenty months. If compared to the average survival of more than ten years after the heart transplantation (1), the benefits of this operation appear self-explanatory. The second example is renal failure. A typical patient with chronic kidney failure must undergo three dialysis sessions per week. However, in the modern era, the projected median graft survival for the deceased donors is above 11 years, and for living donors, it is above 19 years, granting freedom from dialysis for this time (2).
The improvements in longevity and quality of life after organ transplantation are jeopardized by a number of reasons. To name the most common, those are graft rejections and numerous side effects of immunosuppression. Graft rejections ultimately lead to the organ failure, while immunosuppressants place the patients at risk of infections, cardiovascular disorders, and cancer. Sophisticated postoperative follow-up protocols have been introduced to address the hazards. Among many activities, they include regular interventions aiming at the early detection of rejections and malignancies.
In this issue of Heart Vessels and Transplantation, Mohamed MSA brought attention to angiogenesis in various scenarios, including the recipients after organ transplantations (3). The author suggested angiogenesis monitoring could be helpful both in the early and late postoperative periods as a part of follow-up screening.
Progressive angiogenesis in the implanted graft shortly after transplantation promotes postischemic recovery and maintains normal organ function. Therefore, diminished angiogenesis activity could serve as an early marker of graft failure. This pathophysiological axis is evidently most crucial in the first weeks to months postoperatively. Although the message appears clear, when trying to address it in practice, numerous obstacles must be kept in mind. For instance, some traditional markers of angiogenesis, such as vascular endothelial growth factor (VEGF) are actually proinflammatory, overlapping with rejection. In other words, interpretation of isolated VEGF levels may be misleading.
Conversely, persisting high angiogenesis activity in the long term after transplantation may suggest the development of cancer. This aspect should draw attention beginning from the second post-transplantation year. Again, practical assessment may be not straightforward. For instance, elevated VEGF blood level after cardiac transplantation is a strong marker of chronic coronary vasculopathy, which means the specificity of this marker for malignancy in the cardiac recipients will be low.
In the view of the existing challenges of practical assessment of angiogenesis activity via blood-based assays, Mohamed MSA (3) conducted a narrative search to identify its markers and performed in vitro experiments on cell lines.
The investigator concluded that four mediators need to be checked to assess the angiogenetic profile: VEGF, endothelin-1, nitric oxide synthase trafficking inducer (Nostrin), and endothelial nitric oxide synthase (eNOS). With this approach, both the pro- and anti-angiogenic sides of the continuum would be taken into account with potentially robust conclusions.
Clinical studies need to demonstrate if the suggested approach in post-transplantation patients can help in the detection of unwanted early and late pathophysiological patterns.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: V.P.
Acknowledgement and funding: None to declare
Statement on A.I.-assisted technologies use: Author stated that he did not use AI-assisted technologies in preparation of this manuscript
Availability of data and material: Not applies
References
| 1.Khush KK, Cherikh WS, Chambers DC, Harhay MO, Hayes D Jr, Hsich E, et al; International Society for Heart and Lung Transplantation. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-sixth adult heart transplantation report - 2019; focus theme: Donor and recipient size match. J Heart Lung Transplant 2019; 38: 1056-66. doi: 10.1016/j.healun.2019.08.004 https://doi.org/10.1016/j.healun.2019.08.004 PMid:31548031 PMCid:PMC6816343 |
||||
| 2.Poggio ED, Augustine JJ, Arrigain S, Brennan DC, Schold JD. Long-term kidney transplant graft survival-Making progress when most needed. Am J Transplant 2021; 21: 2824-32. doi: 10.1111/ajt.16463 https://doi.org/10.1111/ajt.16463 PMid:33346917 |
||||
| 3.Mohamed SA. A potential innovative surrogate marker for hypoxic injury: Shehata marker of angiogenesis. Heart Vessels Transplant 2025; 9: doi: 10.24969/hvt.2025.540 https://doi.org/10.24969/hvt.2024.540 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

