Answer to quiz on page 26 and Case Discussion: The ICD patient with chest pain
QUIZ
Answer to quiz on page 26 and Case Discussion: The ICD patient with chest pain
Article Summary
- DOI: 10.24969/hvt.2018.55
- Page(s): 29-30
- OPINIONS, DISCUSSIONS, DEBATES
- Published: 19/03/2018
- Received: 18/03/2018
- Accepted: 19/03/2018
- Views: 9458
- Downloads: 8213
- Keywords: quiz, electrophysiology, ICD
Address for Correspondence: Jonathan Lipton,
Royal Hobart Hospital, Hobart, TAS, Australia
E-mail: jonathan.lipton@ths.tas.gov.au
Answers to quiz on electrophysiology and case discussion
Answer to quiz on page 26 and Case Discussion: The ICD patient with chest pain
Question 1. Correct answer C: A 12-lead electrocardiogram.
Chest discomfort has multiple causes. The timing of the symptoms after device implantation suggests a complication of the procedure. Pneumothorax and lead perforation need to be excluded, however an ECG should be performed first as this can be done with minimal delay and can exclude an acute coronary syndrome. Chest X-ray should also be performed and can show pneumothorax, lead dislodgement (however, it is non-specific in detecting perforation), and rib fractures (this patient had received chest compressions during his cardiac arrest). Device interrogation should be performed and can give information on lead dislocation or perforation (increased impedance and thresholds, decreased sensing, and stimulation of extracardiac tissue in the case of a perforation). An echocardiogram should be performed if perforation is suspected to evaluate the presence of pericardial effusion and tamponade. There should be a low threshold for performing a chest CT as this may show a pneumothorax that is not present on echocardiography or lead perforation that is not present on echocardiogram.
Question 2. Correct answer D: Percutaneous revision of ICD lead in operating theatre with cardiothoracic back-up available.
The image clearly demonstrates a perforation of the ICD lead through the anterior interventricular groove and touching the chest wall. Treatment for pericarditis can be started only when clinical findings are consistent with the diagnosis and if lead perforation has been excluded. In this case conservative management would put the patient at risk of developing pericardial effusion and tamponade but also lead dysfunction that could result in both undetected arrhythmia and inappropriate ICD shocks. Urgent intervention is indicated in the case of tamponade and may require emergency pericardiocentesis or thoracotomy to treat tamponade and cover the perforation. In this case, lead revision is appropriate with retraction of the lead into the heart and repositioning with periprocedural echocardiographic monitoring for development of pericardial effusion; surgical backup should be present to perform thoracotomy without delay if needed.
Discussion
Our patient suffered an out-of-hospital cardiac arrest while dining at a local eatery. He received immediate and effective cardiopulmonary resuscitation (CPR), by a trained medical professional, who happened to be at the scene at the time of the arrest. Spontaneous circulation returned after 23 minutes and in this process he sustained sternal and multiple rib fractures. The pain had been managed adequately with medications and the symptoms he had the night of implantation, were located to the left lateral chest wall. The 12 lead ECG was normal, the chest X-ray did not show a pneumothorax and the lead positions were unchanged from directly after the procedure (Fig. 2). An urgent echocardiogram was performed and did not show pericardial effusion, the lead tip appeared to be within the myocardium. Device interrogation was performed with satisfactory ventricular sensing, normal impedance and pacing thresholds. It was noted that there was a chest wall ‘twitching’ during the ventricular pacing threshold test at higher output. This finding was strongly suggestive of a lead perforation with the tip electrodes capturing the chest wall musculature. The CT of the chest confirmed the diagnosis showing a perforation of the ICD lead through the anterior interventricular groove and the epicardial fat and almost touching the chest wall.
Subsequently, lead extraction and repositioning was arranged for the next day. The procedure was performed in the operating theatre, with a general anesthetic and transesophageal echo monitoring for pericardial effusion and a cardiothoracic surgery team available on stand-by. The patient was prepared for a possible sternotomy.
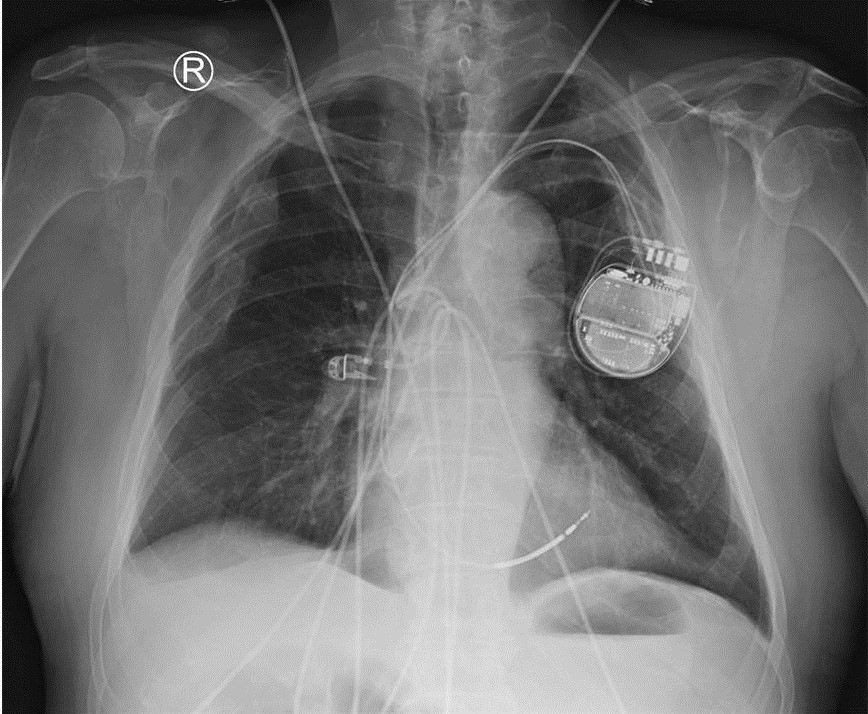
Figure 2. Chest X-ray.
The previous incision was opened, generator extracted from the pocket and leads disconnected. A stylet was inserted in right ventricular (RV) lead and the helix was retracted. Light traction was applied to the lead until the tip was back inside the heart. The lead was then repositioned in low-septal RV position and fixated. Good lead parameters were obtained. On echo a small amount of pericardial effusion developed approximately 10 min after the lead retraction, but remained stable for 30 minutes after the procedure retraction. No signs of tamponade were observed and the patient was returned to recovery. Transthoracic echocardiography the next 2 days did not show any change in pericardial effusion. The patient remained well and was safely discharged home.This case highlights the importance recognizing subtle clinical signs in patients after cardiac device implantation as they may indicate a complication. In this case, the cardiac physiologist recognized signs of extracardiac stimulation as possible lead perforation. The subtle chest discomfort could have been missed or presumed to be secondary to musculoskeletal chest pain. Cardiac device implantation has an overall complication rate of 3-7%. The risk of lead perforation ranges from less than 1% to nearly 6% (1). A cohort study of asymptomatic patients demonstrated a prevalence of 6% by CT, though usually without clinical consequence (2).
Clinical presentation may be non-specific, including pain, device malfunction, phrenic or chest wall stimulation, hemothorax and tamponade (1). The importance of the multiple imaging modalities including CT is clearly defined in this case, as chest radiograph and transthoracic echo are often non-revealing of the complication (3).
Though large studies are lacking, reported risk factors for perforation include older age, female gender, ICD lead, active fixation lead, free wall or apical lead position, and steroid use (4).
No guidelines exist on the best approach to manage acute lead perforation, however, guidelines for chronic lead extraction recommend a multidisciplinary approach in its management, involving the cardiothoracic team, performing the procedure in a setting that allows emergency intervention in case of tamponade (5,6).
In summary, this case illustrates the importance of careful clinical evaluation of a patient with symptoms after a cardiac device implantation and relying on multiple testing modalities to recognize acute lead perforation. A perforated lead can usually be repositioned without major complications but should be performed with a cardiothoracic team on stand-by.
Dolly Marope1, Ashutosh Hardikar1, Keshav Bhattarai1, Jonathan A. Lipton1,2
1Royal Hobart Hospital, Australia
2University of Tasmania, Australia
Peer-review: Internal
Conflict of interest: None to declare
Authorship: D.M., A.H., K.B., J.A.L. contributed equally to preparation of quiz and case report
Acknowledgement and funding: None to declare
Ethics: Informed consent was obtained from patients before all procedures
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

