Pattern of coronary artery disease and its correlation with risk factors and severity of disease in patients with established peripheral artery disease: Doppler and angiographic study
ORIGINAL RESEARCH ARTICLE
Pattern of coronary artery disease and its correlation with risk factors and severity of disease in patients with established peripheral artery disease: Doppler and angiographic study
Article Summary
- DOI: 10.24969/hvt.2024.552
- CARDIOVASCULAR DISEASES
- Published: 15/03/2025
- Received: 27/11/2024
- Revised: 21/01/2025
- Accepted: 25/01/2025
- Views: 4362
- Downloads: 2379
- Keywords: Ankle brachial index, coronary artery disease, cardiovascular risk, peripheral artery disease, SYNTAX score, TASC II classification
Address for Correspondence: Riyaz Charaniya, Department of Cardiology, U.N. Mehta Institute of Cardiology and Research Centre Ahmedabad-380016, India
Phone: +91 8849951109 Email: riyaz.doc@gmail.com
ORCID: Tarunkumar Madan – 0009-0005-2119-2712; Dinesh Joshi - 0000-0003-2723-6227; Riyaz Charaniya – 0000-0002-9330-987X; Krutika Patel – 0000-0002-8613-6915
Ajinkya Borhade, Tarunkumar Madan, Dinesh Joshi, Riyaz Charaniya, Krutika Patel, Anand Dhakne, Himani Upadhyaya, Parth Thakkar
Department of Cardiology, U.N. Mehta Institute of Cardiology and Research Centre Ahmedabad-380016, India
Abstract
Objective: Peripheral arterial disease (PAD) is one of the underdiagnosed and undertreated vascular disease burden irrespective of symptoms in India. The main of our study to assess the pattern in angiographic coronary artery disease (CAD) and PAD severity using Trans-Atlantic Inter-Society Consensus II (TASC II) in Indian population.
Methods: This prospective observational study includes 500 patients admitted with clinical symptoms suggestive of PAD. Clinical and demographic characteristics, risk factors of CAD and past history were recorded. Ankle brachial index (ABI) and The Trans-Atlantic Inter-Society Consensus II (TASC II) classification (TASC II) score were evaluated for severity of PAD and SYNTAX score was calculated for severity of CAD.
Results: The study, involved predominantly male participants with a mean age of 59.2 years. The study found that 34% of patients had double vessel disease (DVD), 28% had triple vessel disease (TVD), and 22% had single vessel disease (SVD). Findings were consistent across the four PAD TASC II classification subtypes, with increasing severity of PAD linked to greater severity of CAD. Type D patients were mostly seen in moderate (38.5%) and severe (30.8%) SYNTAX score groups. Significant differences were observed in mean SYNTAX scores and reductions in ABI across TASC II subtypes, indicating increased PAD severity (p<0.0001).
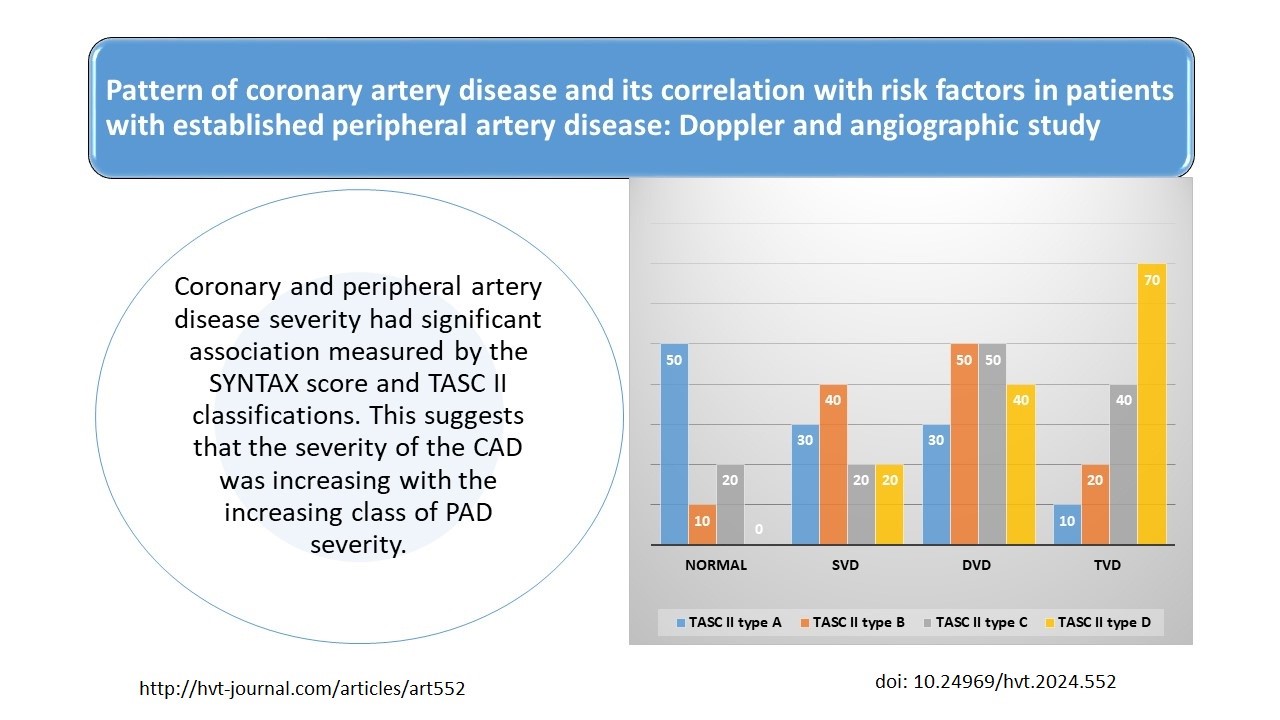
Conclusions: There is a significant association between coronary and peripheral artery disease severity, as measured by the SYNTAX score and TASC II classifications. The severity of the CAD was increasing with the increasing PAD severity.
Key words: Ankle brachial index, coronary artery disease, cardiovascular risk, peripheral artery disease, SYNTAX score, TASC II classification
Graphical abstract
Introduction
Coronary artery disease (CAD) remains a leading cause of morbidity and mortality globally, often intricately linked with peripheral artery disease (PAD) (1) Understanding CAD prevalence and patterns in PAD patients is vital for managing cardiovascular (CV) risks. Doppler ultrasound and angiography are essential tools in assessing these conditions. PAD patients frequently show high rates of concurrent CAD, reflecting the systemic nature of atherosclerosis, with more severe and multi-vessel coronary involvement compared to those without PAD (2). Both conditions share risk factors such as hypertension, diabetes, hyperlipidemia, and smoking.
Past research study`s data suggest that over 50% of PAD patients may exhibit asymptomatic or symptomatic CAD, indicating the necessity for thorough CV evaluation in this group (3-5) Studies indicate that PAD severity often correlates with the extent of coronary disease. Patients with severe PAD, like critical limb ischemia, tend to have extensive coronary artery stenosis. Chronic kidney disease also exacerbates CAD risk in PAD patients. Doppler and angiographic findings often reveal significant coronary artery stenosis, leading to interventions like angioplasty or bypass surgery. Elevated inflammatory markers in PAD patients may further contribute to aggressive CAD (2). Effective management includes lifestyle changes, medication, and regular monitoring.
Risk of death in patients of PAD within 10 years is 4 times more than in those without the disease (4).
The ankle-brachial index (ABI) is an independent predictor of coronary and cerebrovascular outcomes (6). The Trans-Atlantic Inter-Society Consensus II (TASC II) classification assesses PAD based on lesion characteristics, while the SYNTAX score evaluates CAD severity (7, 8).
Our study in Indian population examined the relationship between CAD severity (using the SYNTAX score) and PAD severity (using the TASC II score).
Methods
Study and population
This prospective observational study includes 500 patients admitted with clinical symptoms suggestive of PAD diagnosed with Doppler ultrasonography and peripheral angiography during August 2019 to July 2021 at our tertiary cardiac care hospital. Patients who had past history of PAD and percutaneous coronary intervention or coronary artery bypass surgery were excluded from the study. Patients were divided in the groups according to CAD presence and extent (normal n=80; single-vessel disease, SVD – n=110; double-vessel disease, DVD –n=170; triple-vessel disease, TVD – n=140)and severity of PAD by TASCII classification (TASC II type A – n=120, TASC II type B – n=120, TASC II type C – n=130, TASC II type D– n=130).
Written inform consent was taken from patients or their relative. The study protocol was approved from the institutional ethics committee (UNMICRC/CARDIO/2019/11).
Baseline variables
Data were collected prospectively from 500 consecutive patients using preformed questionnaire. Clinical and demographic characteristics including age; sex; diabetes mellitus, dyslipidemia, hypertension, current and past history of cigarette smoking were recorded. In addition to routine investigations like lipid profile, serum creatinine and HbA1C and left ventricular ejection fraction (LVEF) were measured on admission.
Coronary and peripheral angiography
Coronary angiography data were obtained from the Phillips software system database that includes detailed angiographic findings of all 500 patients. All 500 patients underwent peripheral angiography with coronary artery angiography at the same setting. Obstructive CAD burden was assessed with the help of SYNTAX score and PAD was classified as per TASC-II classification.
Peripheral arterial disease
PAD is a circulatory problem causing a reduced blood flow through the arteries (5). Peripheral angiography was performed trans-radially in majority of patients with a 6-Fr pigtail catheter.
For evaluation of both lower extremities, the catheter tip was positioned above the aorta-iliac bifurcation. TASC II score analysis was performed based on peripheral angiogram. Patients’ were excluded if they had undergone any previous peripheral or coronary artery revascularizations. Based on the findings of the aortoiliac and femoro-popliteal segments, the TASC II classification was used to assess the extension and severity of the disease (9).
The ankle-brachial index
The ABI is a simple, non-invasive test used to diagnose PAD. Blood pressure readings were taken in both arms and ankles. A value less than 0.90 was accepted as indicating PAD.
SYNTAX score
Coronary angiography was performed trans-radially in majority. Each coronary lesion producing 50% diameter stenosis in vessels of diameter 1.5 mm was scored separately and added together to provide the overall SS, which was calculated using the SS score algorithm. The SYNTAX score, a marker for CAD severity, was calculated using specialized software. For comparative analysis the study population was divided into 3 groups on the basis of SYNTAX score (group I (mild): <22, group II (moderate): 22-32, group III (severe): >32) (7).
Statistical analysis
Statistical analysis was performed using the SPSS 26.0 software package (IBM, New York, USA). Continuous variables are expressed as mean (Standard Deviation, SD) and categorical variables are expressed as number and percentage. Differences in two group means or proportions were assessed using independent t-test or Chi-square test as appropriate. Analysis was done to compare the differences among the three groups and to determine the factors predicting the presence and severity of coronary artery score using ANOVA test. Correlation between continuous variables and SYNTAX score was tested using Pearson correlation co-efficient test. A 2-tailed p value <0.05 was considered statistically significant for all analysis.
Results
This prospective observational study had higher prevalence of male (84%) gender. The mean age of the total population was 59.2 (11.6) years. Most of the study population had dyslipidemias (72%) followed by smoking (60%), hypertension (42%) and diabetes mellitus (40%). Most (90%) of the population had normal LVEF (>50%). One third (34%) had DVD, 28% had TVD, 22% had SVD and 16% had normal epicardial vessels. The severe disease was significantly more often seen in males than females (72% vs 12%; p<0.0001). Out of the total population 84% had detected CAD on coronary angiogram. ABI less than 0.9 was seen in 86.6% of the total population. There was an increase in number of risk factors with number of coronary vessels stenosis among the study population The relation of the extent of CAD with clinical variables ABI and patients distribution by TASCII classification are presented in Table 1.
|
Table 1. Relation of TASC-II type and risk factors with number of epicardial coronary vessel stenosis |
|||||
|
Variables |
Normal (n=80) |
SVD (n=110) |
DVD (n=170) |
TVD (n=140) |
p |
|
Age, years* |
47/00 (12.04) |
57 (7.81) |
61.47 (9.04) |
65.21 (10.88) |
<0.0001 |
|
Female, n(%) |
20 (25) |
0 |
10 (5.9) |
50 (35.7) |
<0.0001 |
|
Male, n(%) |
60 (75) |
110 (100) |
160 (94.1) |
90 (64.3) |
|
|
Risk factors |
|
|
|
|
|
|
Hypertension, n(%) |
20 (25) |
30 (27.3) |
70 (41.2) |
90 (64.3) |
<0.0001 |
|
Diabetes, n(%) |
20 (25) |
20 (18.2) |
50 (29.4) |
110 (78.6) |
<0.0001 |
|
Smoking, n(%) |
30 (37.5) |
80 (72.7) |
140 (82.3) |
50 (35.7) |
<0.0001 |
|
Dyslipidemia, n(%) |
20 (25) |
70 (63.6) |
140 (82.3) |
130 (92.9) |
<0.0001 |
|
Mean ABI* |
0.77 (0.16) |
0.74 (0.15) |
0.72 (0.16) |
0.65 (0.16) |
<0.0001 |
|
TASC II type A, n(%) |
50(62.5) |
30(27.3) |
30(17.6) |
10(7.1) |
<0.0001 |
|
TASC II type B, n(%) |
10(12.5) |
40(36.4) |
50(29.4) |
20(14.3) |
<0.0001 |
|
TASC II type C, n(%) |
20(25) |
20(18.2) |
50(29.4) |
40(28.6) |
0.17 |
|
TASC II type D, n(%) |
0 |
20(18.2) |
40(23.5) |
70(50) |
<0.0001 |
|
Data are presented as mean (SD)* and number (%), p<0.05 shows statistical significance ABI- ankle brachial index, DVD- double-vessel disease, SVD – single-vessel disease, TASC II- Trans-Atlantic Inter-Society Consensus Document II TVD- triple-vessel disease |
|||||
![]()
There was statistically significant relation between various risk factors and increase in number of epicardial vessel stenosis (p<0.0001) mentioned in Table 1. Patients with triple-vessel CAD disease were older and male dominated, they had significantly higher rate of risk factors like hypertension, diabetes and dyslipidemia (p<0.0001), markedly lower ABI (p<0.0001) and more severe PAD – TASC II class D (p<0.001).
According to SYNTAX score classification, 70% of population had mild, 18% had moderate and 12% had severe disease. SYNTAX score showed positive correlation with age (r= 0.45; P 0.001) and laboratory findings like HbA1C (r=0.52; p= 0.001), low-density lipoprotein cholesterol (LDL) (0.63; p=0.001), total cholesterol (r=0.57; P 0.001), triglycerides (r=0.57; p=0.001) and negatively correlated with density lipoprotein cholesterol (HDL) (r= -0.51; P 0.001) and ABI index (r= -0.37; p=0.001).
There was almost equal distribution of the study findings among four subtype (A, B, C and D) of PAD TASC II classification (24%, 24%, 26% and 26% , consecutively) (Table 2). Male gender had significantly higher severity of PAD than females (p=0.02). There was increased number of risk factors with subtypes of TASC II classification among study subjects (Table 2).
|
Table 2. Relation of SYNTAX score and risk factors with TASC II types |
||||||
|
Variables |
Total (n=500) |
TASC II type A (n=120) |
TASC II type B (n=120) |
TASC II type C (n=130) |
TASC II type D (n=130) |
p |
|
Age, years* |
59.22(11.57) |
50.50(13.06) |
59.25 (10.41) |
64.08 (7.86) |
62.38 (9.67) |
<0.0001 |
|
Female, n(%) |
80(16) |
20 (16.7) |
10 (8.3) |
20 (15.4) |
30 (23.1) |
0.02 |
|
Male, n(%) |
420(84) |
100 (83.3) |
110 (91.7) |
110 (84.6) |
100 (76.9) |
NS |
|
SYNTAX score, points* |
14.76(12.25) |
4.17 (4.89) |
11.25 (7.8) |
16.92 (11.9) |
25.62 (10.9) |
<0.0001 |
|
Mild, n(%) |
350(70) |
120 (100) |
100 (83.3) |
90 (69.2) |
40 (30.8) |
<0.0001 |
|
Moderate, n(%) |
90(18) |
0 |
20 (16.7) |
20 (15.4) |
50 (38.4) |
<0.0001 |
|
Severe, n(%) |
60(12) |
0 |
0 |
20 (15.4) |
40 (30.8) |
<0.0001 |
|
Risk factors |
|
|
|
|
|
|
|
Hypertension, (%) |
210(42) |
60 (50) |
30 (25) |
60 (46.2) |
60 (46.2) |
0.0002 |
|
Diabetes, n(%) |
200(40) |
10 (8.3) |
40 (33.3) |
70 (35) |
80 (61.5) |
<0.0001 |
|
Smoking, n(%) |
300(60) |
60 (50) |
100 (83.3) |
60 (20) |
80 (61.5) |
<0.0001 |
|
Dyslipidemia, (%) |
370(72) |
10 (8.3) |
100 (83.3) |
120 (92.3) |
130 (100) |
<0.0001 |
|
Mean ABI* |
0.72 (0.16) |
0.83(0.11) |
0.81 (0.11) |
0.63 (0.15) |
0.59 (0.13) |
<0.0001 |
|
Data are presented as mean (SD)* and number (%), p<0.05 shows statistical significance ABI- ankle brachial index, NS – nonsignificant, TASC II- Trans-Atlantic Inter-Society Consensus Document II
|
||||||
There was statistically significant relation between various risk factors and increase severity of PAD (p<0.0001). With increase in severity of PAD there was increase in SYNTAX score CAD severity. Maximum type D patients had moderate (38.5%) and severe 40 (30.8%) SYNTAX score (p<0.0001). When we compare mean SYNTAX score with TASC II types; there was significant difference in mean value of SYNTAX score in relation to subtypes of TASC II –PAD (p<0.0001).
The comparison of mean ABI with TASC II types the mean ABI was reduced with relation to severity of PAD, and there was significant difference in mean value of ABI in relation to subtypes of TASC II -PAD (Pp<0.0001).
Discussion
Patients with peripheral arterial disease have increased CAD because of shared risk factors and common pathophysiology, which is building up of plaques in arterial walls. Previous studies have shown that patients with symptomatic or asymptomatic PAD often present with coronary atherosclerosis and are at increased risk for adverse CV events (4, 5). Aykan et al. (10) found that patients who have more complex peripheral artery lesions also have severe coronary lesions. In Miszalski-Jamka et al. (11) study, computed tomography coronary angiography was proposed to be effective in detecting CAD in subjects with lower-extremity PAD and no cardiac symptoms (11).
Our study was carried out to find out whether the severity of CAD is correlated with severity of PAD as well as risk factors in patients with coronary artery disease.
Our study had higher prevalence of male (78%) above age of 60 years and very few (22%) below age of 60 years, age range was 35-80 years and mean age of 59.2 (11.6) years. Various studies also found same gender and age distribution in their studies (5, 6). Findings of our study correlate with existing literature carried out in different geographical area and also agree that with increasing age there is increase in prevalence of PAD as well as CAD.
The major risk factors were dyslipidemia (72%) and smoking (60%) followed by hypertension (42%) and diabetes mellitus II (40%) (5, 12).
Our findings are also in agreement with results of studies by Vuruskan et al. (8) and Ghosh et al. (13). Grenson et al conducted a large cohort study and found that cardiac disease severity and traditional PAD factors accounted for nearly half of the increased risk of CV morbidity and mortality associated with an incident symptomatic PAD event (14). Several past research studies demonstrated that the ABI is strongly associated with the presence and severity of atherosclerosis in the coronary arteries (8, 13-15). The ABI measurement is considered the most accurate non-invasive diagnostic method when evaluating PAD. In the present study, most of the patients (86.6%) had ABI <0.9.
Male gender, increasing age and smoking conferred a 1.5-fold increased risk for developing PAD (16). Elevated LDL cholesterol and decreased HDL cholesterol were also associated with an increased risk of PAD (12). Our study also supported existing study findings.
In our study, the majority of the patients were male, and the gender predominance increased substantially with increasing TASC II class. Vuruskan et al. (8) and Khanna et al. (17) reported similar to our study findings.
A number of scores have previously been described for grading the severity of CAD on angiography, including the Genisini score, Jenkins score, Syntactic score, and Friesingers score (18). To assess the burden of coronary atherosclerosis, we used the SYNTAX scoring system. We chose this because it is simple, and the SS has been accepted as a CAD burden marker, with predictive usefulness established in a variety of clinical scenarios. After analysing SYNTAX score findings, we discovered that 70% had mild disease, 18% had moderate disease, and 12% had severe disease. In our study, SS increased with higher TASC classes. Our findings are consistent with those of previous studies (7, 8).
Our study identified a significant association between the degree of PAD and the prevalence of 2- or 3- vessel CAD. There was a statistically significant correlation between the SYNTAX score and HbA1c levels (r=0.523,p<0.0001), indicating that higher SYNTAX scores correlate with elevated HbA1c, suggesting poorly controlled diabetes mellitus-II as a risk factor. Elevated HbA1c levels are linked to an increased risk of microvascular and macrovascular diseases (19, 20).
Our findings align with those of Aykan et al. (10), who explored the relationship between PAD and CAD severity in 449 patients. Erkan et al. (7) and Vuruskan et al. (8) also found significant correlations between SYNTAX scores and TASC II classifications, supporting the predictive relationship between CAD and PAD severities.
Our study also showed moderate correlations of the SYNTAX score with age, HbA1c, LDL, total cholesterol, triglycerides, serum creatinine, and negative correlations with LVEF, ABI, and HDL. These findings are consistent with previous studies conducted in different geographic regions (19-21). The inverse correlation between ABI and SYNTAX score suggests that patients with low ABI are likely to have severe CAD, supporting the view that atherosclerosis is a generalized, polyvascular disease.
Study limitations
The main limitations of our study are being a single-centre study and we used only used SYNTAX-I score to correlate severity of CAD with PAD.
Conclusions
There is a significant association between coronary and peripheral artery disease severity, as measured by the SYNTAX score and TASC II classifications. This suggests that the severity of the CAD was increasing with the increasing class of PAD severity.
Ethics: Written informed consent was obtained from all patients and/ or relatives enrolled into the study. The study was approved by the Institutional Ethics Committee (UNMICRC/CARDIO/2019/11)
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: A.B., T.M., D.J., R.C., K.P., A.D., H.U., and P.T. equally contribute to the study and preparation of manuscript, fulfilled all authorship criteria
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: We declare that we did not use AI-assisted technologies in preparation of this manuscript
Data and material availability: Contact authors. Fair use, acknowledgement of authors and sources, and ethics rules apply.
References
| 1.Brown JC, Gerhardt TE, Kwon E. Risk factors for coronary artery disease. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: URL: https://www.ncbi.nlm.nih.gov/books/NBK554410/ | ||||
| 2.Olinic M, Lazar FL, Onea HL, Homorodean C, Ober M, Tataru D, et al. Peripheral artery disease ultrasound assessment in predicting the severity of coronary artery disease. Life (Basel) 2024;14:333. doi: 10.3390/life14030333. https://doi.org/10.3390/life14030333 PMid:38541658 PMCid:PMC10971718 |
||||
| 3.Dhaliwal G, Mukherjee D. Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment. Int J Angiol 2007; 16: 36-44. doi: 10.1055/s-0031-1278244. https://doi.org/10.1055/s-0031-1278244 PMid:22477268 PMCid:PMC2733014 |
||||
| 4.Daoud EM, Ramadan MM, El-Shahhat N, Abd El-Samad AA, El-Malkey N, Sakr SA, et al. Associations of symptomatic or asymptomatic peripheral arterial disease with all-cause mortality and cardiovascular mortality. Egypt Heart J. 2011; 63:7-12. DOI: 10.1016/j.ehj.2011.08.022 https://doi.org/10.1016/j.ehj.2011.08.022 |
||||
| 5.Kumar A, Bano S, Bhurgri U, Kumar J, Ali A, Dembra S, et al. Peripheral artery disease as a predictor of coronary artery disease in patients undergoing coronary angiography. Cureus 2021; 13: e15094. doi: 10.7759/cureus.15094 https://doi.org/10.7759/cureus.15094 |
||||
| 6.Sarangi S, Srikant B, Rao DV, Joshi L, Usha G. Correlation between peripheral arterial disease and coronary artery disease using ankle brachial index-a study in Indian population. Indian Heart J 2012; 64:2-6. doi: 10.1016/S0019-4832(12)60002-9. https://doi.org/10.1016/S0019-4832(12)60002-9 PMid:22572416 |
||||
| 7.Erkan H, Vatan B, Agaç MT, Korkmaz L, Erkan M, Kiris A, et al. Relationship between SYNTAX score and Trans-Atlantic Inter-Society Consensus II classification in patients undergoing diagnostic angiography. Postepy Kardiol Interwencyjnej 2013; 9: 344-7. doi: 10.5114/pwki.2013.38863 https://doi.org/10.5114/pwki.2013.38863 PMid:24570751 PMCid:PMC3927107 |
||||
| 8.Vuruskan E, Saracoglu E, Polat M, Duzen IV. Prediction of coronary artery disease severity in lower extremity artery disease patients: A correlation study of TASC II classification, SYNTAX and SYNTAX II scores. Cardiol J 2017; 24: 495-501. doi: 10.5603/CJ.a2017.0033 https://doi.org/10.5603/CJ.a2017.0033 PMid:28353312 |
||||
| 9.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, Tasc II Working Group. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 2007; 45: S5-67. https://doi.org/10.1016/j.jvs.2006.12.037 PMid:17223489 |
||||
| 10.Aykan AÇ, Hatem E, Karabay CY, Gül İ, Gökdeniz T, Kalaycıoğlu E, et al. Complexity of lower extremity peripheral artery disease reflects the complexity of coronary artery disease. Vascular 2015; 23: 366-73. doi: 10.1177/1708538114550738 https://doi.org/10.1177/1708538114550738 PMid:25208901 |
||||
| 11.Miszalski-Jamka T, Lichołai S, Karwat K, Laskowicz B, Okraska-Bylica A, Wilkosz T, et al. Computed tomography characteristics of coronary artery atherosclerosis in subjects with lower extremity peripheral artery disease and no cardiac symptoms. Pol Arch Med Wewn 2013; 123: 657-63. doi: 10.20452/pamw.2005 https://doi.org/10.20452/pamw.2005 PMid:24185038 |
||||
| 12.Khan A, Khan MG, Khalil IK, Khan S, Khan HA. Correlation of coronary artery disease in patients with peripheral artery disease: cross-sectional study. J Health and Rehabil Res 2024; 4:1490-7. https://doi.org/10.61919/jhrr.v4i1.578 https://doi.org/10.61919/jhrr.v4i1.578 |
||||
| 13.Ghosh S, Mukherjee S, Paul K, Mandal SC. Correlation between severity of Coronary Artery Disease and severity of Peripheral Artery Disease, a detail analytical study from Eastern India. J Cardiol & Cardiovasc Ther 2018; 12: 555841. doi: 10.19080/JOCCT.2018.12.555841 007 https://doi.org/10.19080/JOCCT.2018.12.555841 |
||||
| 14.Grenon SM, Vittinghoff E, Owens CD, Conte MS, Whooley M, Cohen BE. Peripheral artery disease and risk of cardiovascular events in patients with coronary artery disease: insights from the Heart and Soul Study. Vasc Med 2013; 18: 176-84. doi: 10.1177/1358863X13493825 https://doi.org/10.1177/1358863X13493825 PMid:23835937 PMCid:PMC4207208 |
||||
| 15.Nair R, Sud R, Swamy A, Patra V. Unmasking Previously Unrecognized Peripheral Arterial Disease in Patients with Coronary Artery Disease Using Continuous Wave Doppler Using Continuous Wave Doppler Imaging: Does the Presence of Peripheral Arterial Disease Influence the Clinicopathological Profile of Coronary Artery Disease? An Indian Study. Biomed and Biotech Res J 2021; 5: 50-4. doi: 10.4103/bbrj.bbrj_171_20 https://doi.org/10.4103/bbrj.bbrj_171_20 |
||||
| 16.Pabon M, Cheng S, Altin SE, Sethi SS, Nelson MD, Moreau KL, et al. Sex differences in peripheral artery disease. Circ Res 2022; 130: 496-511. doi: 10.1161/CIRCRESAHA.121.320702 https://doi.org/10.1161/CIRCRESAHA.121.320702 PMid:35175843 PMCid:PMC8919803 |
||||
| 17.Khanna NN, Krishna V, Manjunath CN, Tyagi S, Jindal R, Chadha M, et al. The Indian consensus statement for the management of lower extremity peripheral artery disease. J Indian Coll Cardiol 2023; 13: S1-20. doi: 10.4103/1561-8811.383634 https://doi.org/10.4103/1561-8811.383634 |
||||
| 18.Rosmaningtyas CA, Rampengan SH. Coronary angiographic scoring systems to predict prognosis of ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. Intisari Sains Medis 2024; 15: 272-84. doi: 10.15562/ism.v15i1.1953 https://doi.org/10.15562/ism.v15i1.1953 |
||||
| 19.Ascencio AI, Carmona EM, Farías JM, Medina DS, Salas RG, Sauque Reyna L. Prevalence of peripheral arterial disease and principal associated risk factors in patients with type 2 diabetes mellitus: The IDON-Peripheral Arterial Disease Study. Diabetol 2024; 5:190-205. Doi: 10.3390/diabetology5020015 https://doi.org/10.3390/diabetology5020015 |
||||
| 20.Aly K, Sabet S, Elkiey A, Fakhry H. The complexity of peripheral arterial disease and coronary artery disease in diabetic patients: an observational study. Cardiol Res 2023; 14:54-62. doi: 10.14740/cr1463 https://doi.org/10.14740/cr1463 PMid:36896224 PMCid:PMC9990548 |
||||
| 21.Xu W, Guan H, Gao D, Wang Z, Ba Y, Yang H, et al. The association of SYNTAX Score with levels of lipoprotein(a) and inflammatory biomarkers in patients with stable coronary artery disease and different low-density lipoprotein cholesterol levels. Diabetes Metab Syndr Obes 2020;13: 4297-310. doi: 10.2147/DMSO.S279814 https://doi.org/10.2147/DMSO.S279814 PMid:33209043 PMCid:PMC7669512 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

