Organization of the transplantological service on the basis of bioethics in the context of public administration
REVIEW
Organization of the transplantological service on the basis of bioethics in the context of public administration
Article Summary
- DOI: 10.24969/hvt.2025.556
- CARDIOVASCULAR DISEASES
- Published: 25/03/2025
- Received: 22/08/2024
- Revised: 12/02/2025
- Accepted: 15/02/2025
- Views: 3344
- Downloads: 2362
- Keywords: Bioethics, transplantation, surgery, public administration, protection system
Address for Correspondence: Diogena-Halyna Tereshkevych, Department of Ukrainian Studies, Danylo Halytsky Lviv National Medical University, Ukraine
Email: bioethics.ua@gmail.com
ORCID: Diogena-Halyna Tereshkevych - 0000-0003-4427-7872, Olga Dzhura - 0000-0002-0306-44780, Viktoriia Oliferchuk 0000-0003-2800-2254, Lesya Mateshuk-Vatseba -0000-0002-3466-5276
Diogena-Halyna Tereshkevych1a*, Olga Dzhura1b, Viktoriia Oliferchuk2, Lesya Mateshuk-Vatseba1c
1aDepartment of Ukrainian Studies, 1b Department of Histology, Cytology and Embryology, and 1cDepartment of Normal Anatomy Danylo Halytsky Lviv National Medical University, Lviv, Ukraine
2Department of Ecology, National Forestry University of Ukraine, Lviv, Ukraine
Issues of bioethical behavior are crucial in transplantology, because they affect the value and dignity of human life. The previously unsolved part of the general problem is the consideration of the principles of bioethics in solving the problems of transplantation in the context of state policy and the possible directions of the development of legislation based on the principles of bioethics in this area.
The purpose of the article is to analyze state policy in solving transplantation problems from the perspective of bioethics. The proposed study sets the task for public managers to improve regulatory acts in the transplantology, which would be consistent not only with the Constitution, but also with the natural right to life of every person, regardless of the stages and manifestations of his existence, which is a fundamental value of bioethics. Prospects for further research consist in developing measures of public administration bodies to improve the organization of transplantation on the basis of bioethics.
Key words: Bioethics, transplantation, surgery, public administration, protection system
Graphical abstract
Introduction
Transplantation is not exclusively a field of science dealing with problems of transplantation of organs, tissues, or their artificial substitutes. It is the last beam of hope to prolong one's life for a considerable number of people around the world. Every year, approximately 5,000 people need an organ transplant in Ukraine. Some of them go abroad to receive transplants. However, most of individuals die not having undergone the surgery. Therefore, public administration institutions should pay special attention to this area of healthcare and regulate its activity under bioethical principles.
In recent years, the study of the problems of transplantation in Ukraine in the context of public administration has received much attention from both the scientists and practitioners. Among the researchers who studied various aspects of the organization of the transplant service (medical, legal, social), should be singled out Matolinets N, Dubrov S, Samchuk O, Netliukh A. (1), Pishta V. (2), Zborivskyi Y. (3) and others. However, the issues of bioethics in the field of transplantation remained beyond their attention.
The purpose of the article is to analyze state policy in solving transplantation problems from the point of view of bioethics.
The proposed study sets the task for public managers to improve regulatory acts in the field of transplantology, which would be consistent not only with the Constitution, but also with the natural right to life of every person, regardless of the stages and manifestations of his existence, which is a fundamental value of bioethics. Ethical problems of organ transplantation determine three general principles of organ transplantation: protection of the life of the donor and recipient, protection of the identity of the individual and informed consent (4). Prospects for further research consist in the development of measures by public administration bodies regarding the improvement of the organization of transplantation on the basis of bioethics.
Problems and success in transplantology
Transplantation (from Latin translantatio — planting again) is a method of transfer of organs or other materials (tissues) obtained from the donor, and cloned tissues, artificial implants (electronic, metal, etc.) to the recipient (4).
The birth of transplantation dates back to the III century A.D. when Sts. Cosmas and Damian performed a miracle by replacing a sacristan's leg affected by gangrene with the leg of a recently deceased man. Instead, the scientific history of transplantation is much younger; it originated in 1902, when a French pathophysiologist, the Nobel Prize winner in Physiology and Medicine in 1912, Alexis Carrel developed a technique of blood vessel suturing. With this technique, the first heart and kidney transplantations were performed in animals. The greatest obstacle was rejection: the recipient's body rejected foreign tissues and organs.
The 1983 became a crucial year for transplantation when the U.S. Food and Drug Administration approved cyclosporine, which remains the most effective drug against rejection. The discovery provided a strong impetus for the development of organ transplantation surgery and positively affected its success (4).
Nowadays, the medical procedure of organ transplantation has passed an experimental stage and predominantly uses sophisticated therapy for different types of pathology.
The early XX century was marked by the rapid development of clinical transplantation as a highly technological and highly organized area, the use of new methods and approaches in transplantation, and the implementation of transplantation technologies in general surgery.
Every year, June 6 is World Transplant Day. This day is held under the auspices of WHO and is a reminder that thousands of people in the world survived thanks to transplants of organs or tissues.
Annually, over 130 thousand organ transplantations are performed worldwide; for the last 10 years, the number of transplants has increased by 2.5 times. For the last two years, tens of heart transplants have taken place in Ukraine, the lungs and the cornea have been transplanted for the first time, a bone marrow transplantation was done from an unrelated donor, and hundreds of kidney transplants and liver transplants were performed (5).
Transplantation of some organs (for instance, the kidney) was successful. In addition, new perspectives occur in such areas of healthcare, including xenotransplantation (organs or tissues are retrieved from the recipient of other species); the possibility of its clinical use gives hope for recovery to numerous terminally ill patients.
In connection with ethical aspects, annual clinical reality of translation is integrally related to another crucial element, namely "donation of organs", thus, the free decision of a person to give away a part of one's own body (during his/her life or after death) with necessary ethical limits for a person's wellbeing who needs transplants (to safe life of another person without considerable harm to personal life or health). Such an act becomes extremely important both individually and socially, urging society to support the necessity of facilitating the healthcare system and legislative policy while solving the problem of organ search. The lists of patients who need dispositional compatible organs are getting longer in all countries; usually, it is the last chance for survival. For example, in the USA, on average, 14 people die daily while expecting a compatible organ, and approximately the same situation develops in Europe (4).
However, based on public opinion, in theory, almost everybody tends to donate personal organs (after death) for transplantation, while, in practice, most people hesitate to give their consent. There are several factors influencing their decision:
- corruption, crime, in fact, inability to act legally;
- the diversity of terminology used to determine the fact of death ("cerebral", "cardiac", "clinical" and others), and this fact provokes certain misunderstandings;
- the traditional concept of respect towards the body of the deceased as a result of his/her material integrity;
- fear of potential non-objectivity in the death diagnosis of the donor by healthcare personnel and distribution of donated organs;
- the ways to provide personal consent are not always distinct and satisfactory to protect a potential donor's will.
It is necessary to keep in mind the objective complete good of a person, when principles and norms correlate with the human person (6).
Today, transplantation is performed for the kidney, liver, heart, pancreas, lungs, and, recently, intestine; and tissues: cornea, bone tissue, skin, heart valve, and blood vessels. For the last few years, transplantations of entire limbs have been successful (arm, forearm) in some European countries. Such type of intervention demonstrated severe psychological stress on the recipient after such transplantation.
The organs and tissues are obtained "ex cadavere" (from a dead donor) "with a beating heart" or not, or "ex vivente" (from a living donor), depending on the conditions and type of organs or tissues taken for transplantation.
The highest percentage of successful transplantation surgeries was observed during kidney transplantation: after a year the survival rate is 90% in case the transplantation was performed from a living donor, and 82% were done from the deceased; in case of heart transplantation, the survival rate after one year was reached by 83% of patients; lungs transplantations - 74% of patients after one year in case of single transplantation and 86% - in case of dual transplantation; during liver transplantation, the survival rate is up to 80% after one year (7).
The development of transplantology directly depends on the civilization of society. In countries with a high standard of living, this branch of medicine and its legal support are well established, which allows us to transfer this experience to our soil. The bureaucratic management system, which is rooted in medicine, unfortunately, hinders progress in transplantology. But from 2024, within the framework of the medical guarantees program, the state of Ukraine will fully cover the costs of organ transplantation.
The problems of donation and organ and tissue allocation in the context of bioethics
The greatest gift we can give is a gift of ourselves. The same gift can be justified exceptionally with the comprehension of the good as great and decent as, for instance, the life and health of another person. A decision to give a personal part of the body (organs or tissues) without compensation to provide the well-being of the person in desperate need for them is not just an act of altruism or generosity, it is a gesture of demonstration of particular human dignity. This kind of donation is regarded as a true act of love since its performance requires sacrifice of oneself, rather than some possession. Another aspect of deep ethical meaning is related to the issue of donated organ distribution via creating waiting lists or systematization.
Despite direct efforts to foster the culture of organ donation, accessible resources in many countries are insufficient in comparison to the rehabilitation needs of society. Transplantation waiting lists should be compiled based on specific and thorough criteria.
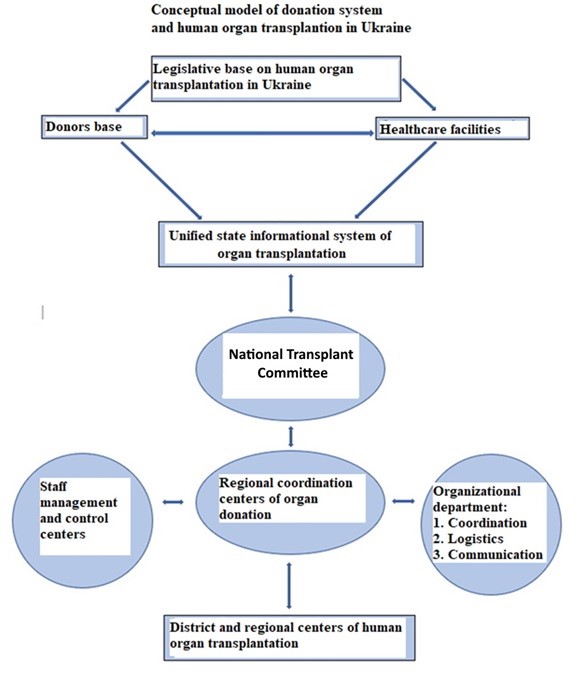
We propose a conceptual model of the organ donation and transplantation system in Ukraine, based on the Law of Ukraine “ On the use of transplantation of human anatomical materials” (Fig. 1).
Ukraine adopted the Law "On Amendments to Certain Laws of Ukraine on Improving the Organization of Medical Care with the Use of Transplantation, and Other Issues in the Field of Healthcare" No. 4203-IХ of 09.01.2025, which entered into force on 08.02.2025 (9). This law improves the process of organ transplantation in Ukraine. Especially, it involves the foundation of the National transplantation committee, that is to consider the cases of unfavorable reactions during transplantation, introduction of the status of urgent transplantation that will meet the needs of patients for urgent transplantation, and also it introduces transplantation based on the domino principle and specifies the conditions of family lifetime donation of anatomical materials.
It prohibits organ harvesting for transplantation from deceased servicemen and casualties of war. The approved legislation amendments will promote the increase in the number of surgeries and saved lives (9).
The ethical principle of righteousness requires the criteria of donated organ distribution not to be grounded on discrimination logic in any possible way (age, sex, nationality, religious beliefs, social background, etc.) or the utilitarian model (capability, social significance, and others). To define priority access to organs for transplantation, it is crucial to thoroughly and fundamentally adhere to immunological and clinical estimates. If these aspects are considered, it is possible to regard a chronological criterion of inclusion of patients on a waiting list. Any other criterion is unjustified and neglects the value of a person (10).
Ethical norms do not allow human organ trade. Regarding the matter of the identity of a recipient, all the above-mentioned ideas on transplantation are relevant to xenotransplantation; the fact of the use of organs or tissues of animal origin does not substantially alternate the stated principles. It is vital to check and evaluate "the stress" caused by such a type of transplantation a patient can receive, and its effect on personal integrity.
It is ethically necessary to ensure thorough and planned monitoring of transplantation subjects which can last even throughout their lives and observation of any possible signal about potential infection by familiar or unfamiliar pathogens.
Besides, each clinical trial has to be carried out in highly specialized centers, with relevant experience in preclinical models (pigs/primates), licensed and regulated by healthcare authorities.
The achieved results should form a positive basis for the dissemination of practicing xenotransplantation as a decisive surgical therapy.
Transplantation and identity of human personality
The conception of "the identity of a person" is multifaceted since there are various philosophical and scientific approaches in this regard (11). We can define "personal identity" as a unity and permanence of a human being about his/her "being and feeling as a person"; it manifests in the historical dimension of a person and his/her communicative structure always via physicality.
It is necessary to stress that personal identity is the good of a person, an inner feature of the existence of a person, and thus, an ethical value that determines the right/duty to promote and protect the integrity of everyone's identity.
In general, we can conclude that implanting a foreign organ into the body of a human being is ethically limited on the level of change it can cause to the identity of the person receiving it (7).
All organs of the human body do not equally demonstrate unique personal identity: some of them perform exclusively their specific function; the others, on the contrary, combine functions into strong and personal symbolic unity, the powers of which depend inevitably on the individual's subjectivity; other organs such as the brain, pituitary gland and gonads are inseparably connected to their function with the personal identity of a subject, independently from their symbolic value. We can conclude that the last ones could not be transplanted since inevitable objective consequences could occur to the recipient or his/her offspring (12). Functional organs and organs with high personal value should be estimated in each particular case, mainly through their symbolic value for a single person (13).
The need to adhere to this ethical principle is essential based on the hypothesis of clinical use of xenotransplantation, i. e. a transplant of organs of animal origin.
The problem of death diagnosis
Death diagnosis is a crucial issue in transplantation. As it was mentioned above, some vital organs can be retrieved only from a dead body. It is necessary to consider one of the questions which is frequently brought up in bioethical debates and it raises public doubts. It is an issue with death diagnosis (6). When a person could be considered dead?
Several decades before, the death diagnosis of a person was quite a simple procedure – death was verified based on the following signs: cessation of heart action and circulation and voluntary breathing, and secondary signs: loss of reflexes including pain sensitivity.
Presently, acquiring new neurological knowledge has caused a change in the actual conception of death: transfer from the concept of death as a precise and sudden "even" (which coincides with the cessation of heartbeat and voluntary breathing) to the concept of death as a "process" which occurs within a certain period starting from "irreversible momentum", thus irreversible disintegration of individual body integration (which coincides with a complete cessation of brain activity), has taken place.
"A person should be considered dead in case he/she lost irreversibly any ability of integration and coordination of physical and intellectual functions of his/her body" (14). Death occurs when a complete cessation of voluntary heart and breathing movements develops, and a complete cessation of brain activity happens (brain death is the correct criterion of death). To make sure, the verification of death is valid, the absence of brain electrical activity is tested with an electroencephalogram (it should not be confused with a coma that is not always irreversible). This method should be done twice within six hours. "Clinical death happens when irreversible cessation of the cerebral cortex and inner parts of the brain responsible for the coordination of activity of organic functions such as breathing, heartbeat, a nerve reflex is stated" (7). The criteria for determination of death are heart, breathing, pulse, reflexes, and brain activity.
Standard criteria of death verification developed by the Medical Department of Harvard University in the USA: complete and irreversible loss of conscience; no response to painful stimuli; complete absence of unconditioned muscular reflexes and inability to stimulate them; broad, dilated unresponsive pupils; complete absence of electroencephalogram waves at least during 6-24 hours (6).
Various terms used for confirmation of the moment of death of a person do not describe different types of death (there are no types of death), but substantiate a single possible fact of the actual death of a person using different methodologies. Therefore, the correct expression is "neurological or brain criteria" of death verification, rather than "brain death"; "heart-circulation criteria", rather than "heart death".
There is the only "death of a person" consisting in the complete and irreversible disintegration of an integrated complex which is a human person in essence, as a consequence of the separation of life principle or spirit and soul of a person from his/her physicality.
Based on its radical sense, the death of a person is an event that cannot be immediately verified either by scientific equipment or empirical method. However, due to scientific progress, it is possible to differentiate biological signs more clearly and in detail, which inevitably accompany the death of a person using the criteria of death verification mentioned before and used by the healthcare industry to technically and scientifically differentiate the moment of death which occurred or is happening now (15).
According to modern scientific research on death verification, the focus from traditional heart and breathing signs was shifted to "neurological" criteria, namely, the identification of complete and irreversible cessation of any brain activity and signs of loss of autointegration of the body. These signs are determined by the majority of the international scientific world. It should be mentioned that the approved Law of Ukraine on organ transplantation (16) is based on this approach/position as well.
While conserved blood for transfusion can be stored in containers for several weeks, and a frozen one – even for a longer period, the organs for transplantation cannot be conserved for so long and can be stored only for several hours. Rapid transplantation is required to be performed immediately, as soon as an organ is retrieved from a donor (6).
Body and brain death does not determine conscience death, the life of a person continues even after the burial of his/her material body under God's watchful who loves each of us and takes care of us and the World where eventually the Universe and everything that is there is pursuing. Our conscience is not a product of the brain, to be more exact, in the time of our existence in our physical body; the brain serves as a temporary vessel of our conscience, which can exist without the brain and even physical body (17).
Informed consent and organ transplantation
Organ donation and transplantation are distinguished by personal and social features, which is why it is ethically necessary to make prior informed consent of both donor and recipient.
Such an act as organ donation requires a donor person to be relevantly informed regarding procedures it includes. In the case of donorship from a living person, he/she has to be properly informed about potential risks and consequences in the future; possible therapeutic and/or preventive measures he/she has to undergo after organ retrieval surgery; dynamics of donated organ distribution. Moreover, it is vital to avoid any psychological pressure or conditions regarding the choice of a donor based on moral, emotional, or, in the worst case, commercial criteria. Only in such a case, he/she can consciously and voluntarily express his/her consent or refusal (18).
In case of organ retrieval from a dead donor, when still alive, he/she has to give consent personally unambiguously for potential donorship of his/her organs. Otherwise, consent from his/her legal representatives is ethically valuable in case it is impossible to learn about the prior choice of the deceased donor directly (19).
General ethical principles of transplantology and their reflection in international and state legislation
Ethical problems of transplantation become more complicated due to the increasing number of people who need organ transplantation, on the one hand, and a lack of proper donors, on the other. Bioethics focuses on the following issues: informed consent of a patient, donor, or his/her relatives; the rights of the society to receive organs from the deceased; inadmissibility of experimental transplantations or such types of transplantations which can affect the identity of a person; verification of death in case of donorship from the dead, and righteousness of donor organs distribution in case of recipients' queue. The crucial factors here are the issues of the relation of technology and ethics and also respect towards the physical nature of an individual. Besides, with the development of technology, the question of transplanting artificial organs or chips imitating human organs becomes relevant.
There is a classification of various forms and types of transplantation in modern science, and it is reflected in international and domestic legislation, considering general ethical principles and particular ethical problems. Based on the Convention on Human Rights (2010), the Council of Europe has launched an active cooperation of the state members in the field of health legislation (18). General and mutual principles for European countries that are the basis for legislation on transplantation are stated in the European Social Charter (1996), which in article 11 obliges the states to take care of the health of their citizens (20), and in European code of social safety (1990) which imposes preventive, treatment and rehabilitation measures (21).
The main principles in the law of the Council of Europe on blood transfusion (code of 1975, Reykjavik), exchange of test on tissues compatibility (Agreement №84 from 1974), issues related to organs transplantations and human tissues and organ retrieval (Recommendation №79/5, Recommendation №78/29 (1978)), aimed at facilitating cooperation and safety in the field of transplantation and prevention of its commercialization (22).
Approval of the European Convention on Bioethics by the Council of Europe was an important event that verified the prohibition of human organ trade (23). However, it includes certain shortcomings and omissions (particularly, it says nothing about the ethically unacceptable use of embryos after abortion).
Organ transplantation and various abuses in this area (trafficking of children, especially of newborn, organ retrieval during surgeries without informing patients, etc.) are relevant problems, and it is described in regulatory documents of all the countries. Organ transplantation is mentioned in 13, 14, and 15 Articles of Principles of European Medical Ethics approved by the International Conference of Medical Professional Associations and Bodies, on January 6, 1987. In October 1987, ХХХІХ Assembly of the World Medical Association approved the Declaration of organ transplantation. The New Italian Code of medical professional ethics (1995) contains two specialized articles (36 and 37) considering the issue of death verification and support of the life of a person defined as clinically dead to prolong the functioning of organs determined for transplantation (4). In Ukraine, a relevant Law was adopted dated 16.07.1999 № 1007-ХІУ "On transplantation of organs and other anatomical materials of a human being". The Law was replaced by the Law of Ukraine "On the use of transplantation of human anatomical materials", which came into force on 01.01.2019 and revealed the issue of organ transplantations. Besides, the Law regulated the transplantation of organs from a dead human body. As of January 1, 2021, according to the Government resolution, the Unified state informational system of organ and tissue transplantation came into action, developed to compile patients’ waiting lists and donor organ lists, and collect information on donor compatibility (5).
In practice, it has been proven that the possibility of transplantation in Ukraine gives rise to its abuse, trafficking in organs or tissues, their forced removal, forced blood donation and even murder for the purpose of transplantation of human organs or tissues.
All of these negative factors create the need for medical and legal regulation of activities related to the transplantation of human organs or tissues. This issue also deserves additional criminal law protection, which in turn necessitates the study of this problem by the science of criminal law (24).
The field of transplantation is regulated by the Constitution of Ukraine (25) and certain provisions of the Civil Code of Ukraine (26). According to the domestic legislation, crimes committed in this area are punishable under Articles 143 and 144 of the Criminal Code of Ukraine of 2001, the disposition of Part 1 of Article 143 of the Criminal Code of Ukraine (27) does not reveal the content of prohibited behavior and is blanket in the way criminal liability is determined. Therefore, in order to thoroughly and accurately clarify the content of the article, it is necessary to refer to:
1) the Law of Ukraine “On Transplantation of Human Organs and Other Anatomical Materials” (8), which regulates the conditions and procedure of transplantation in detail;
2) the fundamentals of legislation of Ukraine on health care of 1992, which serve as a code of medical practice, contain rules that regulate the process of transplantation of human organs and other anatomical materials (28).
They reflect the basic rights of patients during transplantation, the provision of medical care in the critical conditions, general grounds and conditions of transplantation. Ukraine needs to improve the legal framework by defining criminal liability of medical workers who violate the transplantation procedure established by law and abuse their official position, to provide sufficient state funding, as well as to introduce the best practices of European countries in regulating the transplantation of human tissues or organs.
The relevant Law of Ukraine includes ethical limits in the transplantation of organs and other anatomical materials retrieved from humans and animals. Yet, transplantation in the healthcare system of Ukraine has fallen behind in contrast with other countries. The Law does not cover the questions of autotransplantation, implantation, and transplantation of sex organs, reproductive cells, and living embryos (Art. 2; Art. 3). Though, the Law still includes Art. 19, p. 1, according to which "fetal materials for transplantation and/or production of bioimplants are stored in the healthcare facilities which perform surgery of artificial termination of pregnancy (abortion), childbirth and delivery, with signed consent by a woman who provided these materials on the condition that her confidential information is not disclosed which is ethically unacceptable. Authorities have to counter illegal business and cynical trade of parts of human embryos, which are sold abroad (according to the investigative reporting "Closed zone" by the 5th channel in 2004 "Dead, alive, and unborn…").
Demand for donor material has also led to the development of ethically unacceptable ways to receive human transplants accompanied by a wide range of committed crimes such as murder, bodily injury, forgery or destruction of documents, illegal abortion or adoption, commercial agreement regarding a human being, trafficking, malpractice, etc. and socially dangerous acts. It is required to enhance criminal and legal protection of a person; his/her right to safety, life, and health, and define prospective approaches to prevent crime during transplantation. Thus, the Criminal Code of Ukraine establishes legal liability for the procedure of organs and other human anatomical materials transplantation (art. 143) and illegal donorship (art. 144) (27).
Genetic engineering is applied to a person to define individual characteristics such as DNA analysis (paternity, healthy carrier screening for pathogenic genes); to perform therapeutic procedures somatically (treatment of tumor causes is more effective than treatment of consequences); and to intervene in germ cells to prevent the transfer of genetic diseases (DNA is a system of transfer of genetic information of the body, e.g. it may lack genes necessary to produce protein; resist infections, etc.).
Genetic therapy of germ cells is extremely dangerous and ethically unacceptable as it is related to the change of genome in several generations, and can cause unpredictable new mutations and imbalance between human society and the environment.
Embryos production is ethically unacceptable if the aim is to use them as products. Human life begins from the moment of conception and deserves respect (6).
According to regulations, guidelines and public debate in the eight EU member states, embryonic and fetal tissue transplantation (EFTT) and the use of human embryonic stem cells (hES cells) for cell therapy research, including “therapeutic” cloning, are widely used, which is morally unacceptable (29).
However, bioethics based on the principles of personalism draws attention to the biological and anthropological status of the human embryo, which from the moment of fertilization has all the characteristics of a human person: a personal genome-driven project program of life and development and human dignity that deserves respect.
Personalistic bioethics asserts that a human being should be respected and treated as a person from the moment of fertilization, and therefore from that moment on, he or she has the rights of a person, first and foremost, the inviolable right to life, as well as to unconditional respect for his or her dignity in spiritual, mental and bodily integrity. Procedures that involve the manipulation and destruction of human embryos are morally unacceptable, even if they are aimed at a good cause.
Science should look for other ways of treatment that do not involve either cloning or embryonic cell harvesting. It is enough to obtain cells from adult organisms for this purpose or from umbilical cord blood. These are the ways in which research should be directed if we want to preserve the dignity of every human being, starting from the moment of fertilization (4).
General principles, that determine ethical problems of organ transplantation, can be defined as the following three: protection of the donor's and recipient's life, protection of personal identity, and informed consent.
There are three criteria in the medical field for choosing patients for organs transplantation:
- Utilitarian, according to which organs are distributed based on the principles of social utility, thus a patient has an advantage if he/she can return to work, which is ethically unacceptable;
- Randomization criterion, which includes any other motives besides the usual order of transplantation requests;
- Therapeutic, which is the most humane since it considers transplantation urgency, patient's condition, potential success, perspectives of organ engraftment, etc. While any discrimination of a patient is excluded (30).
Organ donation for the benefit of science by will has always been highly valued in medical universities in Europe, as the Anatomical museum of the Department of Normal Anatomy located in the Danylo Halytsky Lviv National Medical University presents >2000 specimens that represents comparative, developmental, gender, systemic, dynamic, plastic, and descriptive anatomy (31).
The progress of transplantation depends on the development of knowledge in this field and the use of the potential technologies that allow us to "unify" tissues and determine the level of their compatibility.
Conclusion
Ethical problems of organ transplantation are defined by three general principles of organ transplantation: protection of the donor's and recipient's life, protection of personal identity, and informed consent.
It is critical to resolve ethical, moral, and social issues regarding organ provision and methods of their distribution on the legislative level, and problems related to the use of living donors as volunteers based on bioethical principles.
Verkhovna Rada of Ukraine should make amendments to the Law of Ukraine "On the use of transplantation of human anatomical materials" (from 17.05.2018 № 2427-VIII ), especially to exclude ethically unacceptable article 19 "Fetal materials for transplantation and/or production of bioimplants are stored in the healthcare facilities, which perform surgeries of artificial termination of pregnancy (abortion), birth and delivery, based on written consent of a woman as a result of whose pregnancy these materials were obtained, on the condition of confidentiality of her personality", and to improve the functioning of transplantation service.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: D-H.T., O.D., V.O., and L.M-V.
equally contributed to the study and preparation of manuscript, fulfilled all authorship criteria
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: Authors declare they did not use AI-assisted technologies in preparation of this manuscript
Data and material availability: Contact authors. Fair use, acknowledgement of authors and sources, and ethics rules apply
References
| 1.Matolinets N, Dubrov S, Samchuk O, Netliukh A. Practical aspects of organ transplantation based on the regulatory documents and clinical practice at the communal non-profit enterprise "Lviv Clinical Emergency Hospital". Pain, Anaesthesia & Intensive care 2020; 4: 22-30. Doi: 10.25284/2519-2078.4(93).2020.220654 https://doi.org/10.25284/2519-2078.4(93).2020.220654 |
||||
| 2.Pishta VI. Legal aspects of transplantation of anatomical materials from a minor donor. Vcheni Zapysky TNU imeni V.I. Vernadskoho. Seriia: Yurydychni Nauky 2020; 31: 31-5. Doi: 10.32838/TNU-2707-0581/2020.5/06 https://doi.org/10.32838/TNU-2707-0581/2020.5/06 |
||||
| 3.Zborivskyi YY. Civil liability in the field of transplantation of human anatomical materials. Yurydychnyi Naukovyi Elektronnyi Zhurnal 2023; 2: 140-2. Doi:10.32782/2524-0374/2023-2/30 https://doi.org/10.32782/2524-0374/2023-2/30 |
||||
| 4.Tereshkevych HT. Fundamentals of bioethics and biosafety. Ternopil, Ukraine; Press TDMU: 2018. 400p. (In Ukranian) | ||||
| 5.Kuryshko D. Will Ukraine say "yes" to organ donation? 2021. Available at: URL: https://www.bbc.com/ukrainian/features-58756985 (Accessed 03 January 2022), Ukraine. | ||||
| 6.Sgreccia E. Manuale di bioetica. vol. I. Milano, Italy; Vita e Pensiero: 2012: 1016p. | ||||
| 7.Nuova Carta degli Operatori Sanitari. Pontificio Consiglio per gli Operatori Sanitari (per la Pastorale della Salute). Vaticano; Libreria Editrice Vaticana Città del: 2016. 152p. (accessed 29 July 2024.) Available at: URL: https://www.humandevelopment.va/content/dam/sviluppoumano/pubblicazioni-documenti/documenti/Nuova%20Carta%20Operatori%20Sanitari%20-%20IT.pdf | ||||
| 8.VRU (2018). Law of Ukraine "On Application of Transplantation of Anatomical Materials to Man", 2018. No. 2427-VIII / Information of the Verkhovna Rada of Ukraine. 2018, № 28, Art. 232. Ukraine. | ||||
| 9.VRU (2025). Law of Ukraine "On Amendments to Certain Laws of Ukraine Regarding Improvement of the Organization of Medical Care with the Use of Transplantation, Other Issues in the Field of Healthcare", which entered into force on 08/02/2025, dated 09.01.2025 No. 4203-ІХ / Information of the Verkhovna Rada of Ukraine. 10.01.2025. Ukraine. | ||||
| 10. Kalipari M. Bioethics and organ transplantation. In: Anthology of bioethics. Ed. Yu. I. Kundiev. Lviv, Ukraine: BaK; 2003: pp. 336-348. (In Ukranian). | ||||
| 11. Grinberg L, Grinberg R. Identità e cambiamento. Roma, Italy; Armando: 1992. 272p. | ||||
| 12. Faggioni MP. Transplantation of gonads and current situation. Medicina e Morale 1998; 47: 15-46. DOI:10.4081/mem.1998.840 https://doi.org/10.4081/mem.1998.840 |
||||
| 13. Cuer P. Quelques considérations éthiques, notamment sur lidentité lors de xénotransplantations. Path Biol 2000; 48: 426-8. | ||||
| 14. VRU (2013). On establishing diagnostic criteria for brain death and procedures for determining the moment of death of a person: Order of the Ministry of Health of Ukraine dated 23.09.2013, No. 821. Available at: URL: http://zakon.rada.gov.ua/laws/show/z1757-13, (Accessed 03 Jan 2022). Ukraine. | ||||
| 15. Giovanni Paolo II. Discorso ai partecipanti al XVIII Congresso Internazionale della Transplantation Society. 28 Agosto 2000. Roma, Italy: Avvenire; 2000. r.2-4. | ||||
| 16. VRU. Law of Ukraine "On transplantation of organs and other human anatomical materials"of 16.07.1999 No. 1007-XIU // Bulletin of the Verkhovna Rada of Ukraine. 1999. № 41. Art. 377. - Expired on the basis of: VRU (2018), Law of Ukraine "On Application of Transplantation of Anatomical Materials to Man", 2018. No. 2427-VIII / Information of the Verkhovna Rada of Ukraine. 2018, № 28, Art. 232. Ukraine. | ||||
| 17. American neurosurgeon: the death of the body and the brain does not mean the death of consciousness. 2015. Available at: https://goneva.net.ua/vsyachina/4805-amerikanskiy-neyrohirurg-smert-organizma-i-mozga-ne-oznachaet-smert-soznaniya.html (Accessed 03 January 2022). (In Ukranian). | ||||
| 18. Fisichella R (editor). Catechismo della Chiesa Cattolica. Testo integrale e commento teologico. Casale Monferrato; PIEMME: 1993. 1280p. | ||||
| 19. European Convention for the Protection of Human Rights and Fundamental Freedoms 4.XI.1950. Rome, Italy. Available at: URL: www.hri.org/docs/ECHR50.html. (Accessed 03 January 2022) | ||||
| 20. European Social Charter, 1961, revised by the Council of Europe. Strasbourg, May 3, 1996. Available at: URL: www.coe.int/T/E/Human_Rights/Esc/ (Accessed 03 January 2020) | ||||
| 21. European Social Security Code (1990) (revised) (ETS N 139) Rome, 6 November 1990. Available at: URL: https://zakon.rada.gov.ua/laws/show/994_651#Text (Accessed 03 January 2022). | ||||
| 22. Torrelli M, Guiran J. Le médecin et les droits de lhomme. Paris: Bergrr-Lévrault: 1983: 466p. | ||||
| 23. Convention on the Protection of Human Rights and Dignity in the Application of Biology and Medicine, 1997 CE. Available at: URL: conventions.coe.int/Treaty/EN/Treaties/Html/164.htm (Accessed 03 jan 2022). | ||||
| 24. Barsuchenko Y.O. Criminal and legal problems of transplantology in Ukraine: ways of their solution and prospects for development. Information and Law 2018; 2: 177-82. | ||||
| 25. VRU (1996). "Constitution of Ukraine". Available at: URL: http://zakon5.rada.gov.ua/laws/show/en/254%D0%BA/96-%D0%B2%D1%80 (Accessed 03 January 2025) | ||||
| 26. VRU (2003). "Civil Code of Ukraine". Lists of the Verkhovna rada of Ukraine. vol. 40-44, Art. 356. | ||||
| 27. VRU (2001). "Criminal Code of Ukraine", Lists of the Verkhovna Rada of Ukraine, vol. 25-26. | ||||
| 28. VRU (1992), Fundamentals of the legislation of Ukraine on health care: Law of Ukraine of 19.11.1992 № 2802-XII / Information of the Verkhovna Rada of Ukraine. Ukraine. | ||||
| 29. de Wert G, Berghmans RL, G J Boer, S Andersen, B Brambati, A S Carvalho, K Dierickx, S Elliston, P Nunez, W Osswald, M Vicari. Ethical guidance on human embryonic and fetal tissue transplantation: a European overview. Med Health Care Philos. 2002;5(1):79-90. DOI: 10.1023/a:1014213125573 https://doi.org/10.1023/A:1014213125573 PMid:11954997 |
||||
| 30. Nanni G. Microallocazione delle risorse: il punto di vista del chirurgo / a cura di E. Sgreccia, A. Spagnolo. Etica allocazione della risorse in sanitá. Milano: Vita e Pensiero. 1996: 148-156. | ||||
| 31. Pidvalna U., Mateshuk-Vatseba L. Mortui vivos docent [The dead teach the living]. Journal of Morphological Sciences 2019; 36(04): 291-294. DOI: 10.1055/s-0039-1698377 https://doi.org/10.1055/s-0039-1698377 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER