Sternoclavicular osteomyelitis with hematogenic dissemination: A case report
CASE REPORT
Sternoclavicular osteomyelitis with hematogenic dissemination: A case report
Article Summary
- DOI: 10.24969/hvt.2025.603
- CARDIOVASCULAR DISEASES
- Published: 31/10/2025
- Received: 18/08/2025
- Revised: 13/10/2025
- Accepted: 14/10/2025
- Views: 1069
- Downloads: 944
- Keywords: Osteomyelitis, sternoclavicular joint, Staphylococcus aureus, diabetes, hypertension
Address for Correspondence: Nara Gomes Ahmed, Mayor Dulcidio Cardoso Avenue, 1400, Block 2, Apartment 1703; Barra da Tijuca, Rio de Janeiro – RJ, Brazil, Zip Code: 22620-311
E-mail: naragomesahmed@gmail.com Phone: +55 21982209983
ORCID: Nara Gomes Ahmed –0009-0002-6892-320X; , Bruno Cordeiro Zappa - 0000-0003-0226-9313, Odenice Souza Souto-0009-0002-9244-5746, Carla Manuela Aparecida Leitão Ribeiro - 0009-0006-9618-9275, Lara Patricia Lopes de Castro Osorio 0009-0008-0870-8050, Juliana Ribeiro Braga - 0000-0002-7883-2216, Brenda Kriscya Clem Pinheiro- 0009-0000-2730-1223
Nara Gomes Ahmed1a*, Bruno Cordeiro Zappa2, Odenice Souza Souto1a, Carla Manuela Aparecida Leitão Ribeiro1b, Lara Patricia Lopes de Castro Osorio1a, Juliana Ribeiro Braga1a, Brenda Kriscya Clem Pinheiro1a
1aSilvestre Adventist Hospital, 1b Department of Clinical Medicine, Silvestre Adventist Hospital, Rio de Janeiro - RJ, Brazil
2National Institute of Cardiology, Silvestre Adventist Hospital, Rio de Janeiro - RJ, Brazil
Abstract
Objective: Sternoclavicular osteomyelitis is a rare and serious infection, mainly caused by bacteria, which can result in hematogenous spread even in the absence of a prior adjacent infection.
We report the case of a patient with hematogenous sternoclavicular osteomyelitis, highlighting the clinical progression from nonspecific initial symptoms to the definitive diagnosis, as well as the multidisciplinary therapeutic approach employed.
Case presentation: A 64-year-old male patient was admitted after experiencing progressive pain in the left shoulder, which evolved into a painful sternoclavicular nodule, accompanied by fever and weight loss. The diagnosis confirmed methicillin-sensitive Staphylococcus aureus sternoclavicular oste omyelitis, isolated from the surgically removed abscess. The patient received intravenous antibiotic therapy and multidisciplinary support, with clinical and laboratory improvement. Hospital discharge was planned after transitioning to oral therapy.
Conclusion: Sternoclavicular osteomyelitis presents with nonspecific symptoms that make diagnosis challenging and requiring accurate testing for appropriate treatment.
Key words: Osteomyelitis, sternoclavicular joint, Staphylococcus aureus, diabetes, hypertension
Introduction
Sternal osteomyelitis is a rare but potentially severe infection, accounting for only 0.51% of all septic arthritis cases (1, 2). Primary hematogenous osteomyelitis occurs when bacteria circulating in the bloodstream localize in the sternum, leading to
infection. This form is even rarer and can develop in
the absence of apparent infection at other sites in the body (3). Primary sternal osteomyelitis occurs without an adjacent infected site, unlike the secondary form, which typically arises as a complication of sternotomy (4).
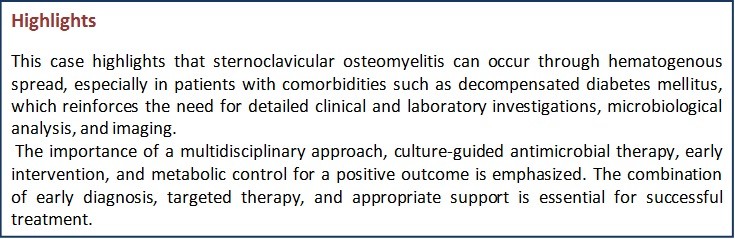
Graphical abstract
Sternal osteomyelitis may present with chest pain, fever, swelling, and localized tenderness. However, not all these symptoms are always present, which can hinder diagnosis and lead to confusion with cardiac or pulmonary conditions. This may delay treatment initiation, worsening the clinical course (2).
Risk factors include intravenous drug use, diabetes, and obesity (1, 5). The most common bacterial cause of sternal osteomyelitis is Staphylococcus aureus, although Pseudomonas aeruginosa is frequently identified in intravenous drug users (2).
The diagnosis should be suspected in patients with acute inflammatory swelling over the sternum. It is further confirmed by leukocytosis, elevated erythrocyte sedimentation rate, lateral radiography of the sternum and a positive Gram stain (6). Imaging tests such as computed tomography (CT) and magnetic resonance imaging (MRI) are essential to confirm suspected cases, even when radiological findings appear late in the course of the disease (2).
In most cases, treatment involves antibiotics alone. However, in more complex situations, antibiotic therapy may need to be combined with surgical debridement and soft tissue reconstruction using vascularized flaps to ensure adequate coverage of the affected area (1, 5).
In this context, we report the case of a patient with hematogenous sternoclavicular osteomyelitis, highlighting the clinical progression from initial nonspecific symptoms to the definitive diagnosis, as well as the multidisciplinary therapeutic approach employed.
Case report
A 64-year-old male patient was admitted to the Inpatient Unit on October 19, 2024, seeking medical attention due to progressive pain in the left shoulder, initially diagnosed as bursitis. Over time, the pain worsened and migrated to the anterior chest region, accompanied by a painful nodule in the sternal notch, persistent fever, and significant weight loss (approximately 10 kg over the preceding months). The discomfort intensified when lying down, impairing sleep and breathing, which led to hospital admission.
Upon admission, the patient appeared well but presented a 4 cm painful nodule in the sternoclavicular region, tender to palpation, without surrounding edema. Upon admission, the patient was lucid, oriented, acyanotic, anicteric, eupneic on room air, and afebrile to the touch.
Cardiac auscultation revealed a regular rhythm, normal heart sounds, and no murmurs. Respiratory auscultation revealed a universally audible breath sound, with the presence of a nodule in the left sternoclavicular joint. The abdomen was soft, peristaltic, tympanic, and painless to palpation. The lower limbs presented edema and hyperemia. Signs included a temperature of 37-35°C, heart rate of 102-76 bpm, respiratory rate of 24-17 breaths per minute, blood pressure ranging from 184/110 to 97/70 mmHg, and oxygen saturation of 98-93%. He had a recent history of hypertension and decompensated diabetes (capillary blood glucose ranging from 262 to 439 mg/dL). He was taking metformin for diabetes, enalapril for hypertension, and simvastatin for dyslipidemia. The differential diagnosis included osteosarcoma, prostate cancer with bone metastasis, and mediastinitis.
Laboratory findings showed hemoglobin (Hb) 10.3 g/dL, leukocytes 16,110/µL (60%), platelets 603,000/µL, potassium (K) 5.4 mmol/L, phosphorus (P) 3 mg/dL, C-reactive protein (CRP) of 6.3 mg/dL, erythrocyte sedimentation rate of (ERS) 100 mm/h, hematocrit of 30.4%, sodium (Na) 135 mmol/L, creatinine (Cr) 0.6 mg/dL, urea (Ur) 25 mg/dL, magnesium (Mg) 2.1 mg/dL. The 24-hour blood glucose record showed persistently high values: 322 mg/dL at 10:00 AM (8 IU of regular insulin), 323 mg/dL at 9:00 PM (8 IU of regular insulin), and 322 mg/dL at 6:00 AM (2 IU of regular insulin).
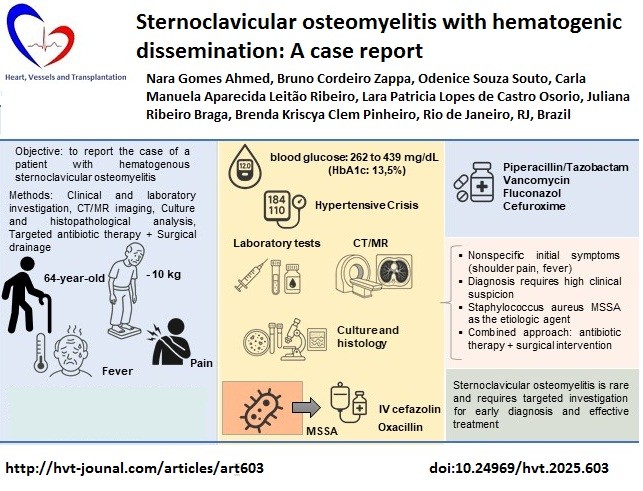
Imaging and laboratory tests indicated an infectious process in the anterior mediastinum, initially interpreted as cellulitis, which progressed to a sternoclavicular abscess. A chest CT scan revealed fat stranding in the mediastinum, narrowing of the right sternoclavicular joint space, heterogeneous attenuation of the muscle planes, and small cystic collections with abscess formation (Fig. 1).
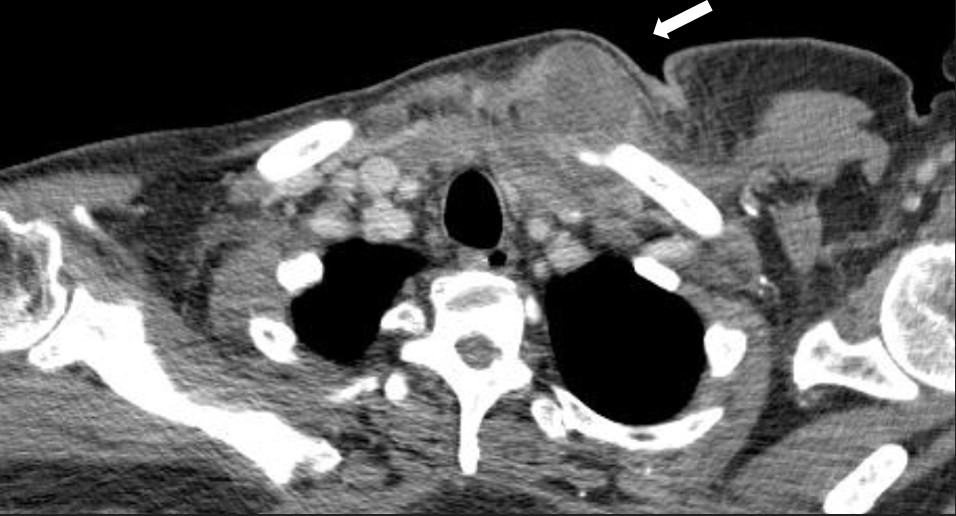
Figure 1. Computed axial tomography. Diffuse bone edema with soft tissue edema also characteristic of osteomyelitis.
MRI of the chest showed findings consistent with osteomyelitis, including bone irregularities, edema, subchondral erosions of the right sternoclavicular joint, synovitis, and inflammatory joint changes (Fig. 2- 4).
Surgical drainage of the abscess was performed, with a favorable initial response. Material was sent for culture and histopathology analysis. On the third day of hospitalization, cultures identified methicillin-sensitive Staphylococcus aureus (MSSA). Histopathology revealed a benign lesion, and tests for AFB (acid-fast-bacili), GeneXpert for M. tuberculosis, direct microscopy for fungi, and mycobacteria were negative, ruling out tuberculosis and other infectious causes. An image-guided biopsy showed no signs of malignancy. Based on the clinical and laboratory findings, the diagnosis of hematogenous sternoclavicular osteomyelitis was confirmed by the medical team.
During hospitalization, the patient used different antimicrobials regimens as his condition evolved. Initially, he was treated with piperacillin/tazobactam (from the 1st day to the 5th day of hospitalization), vancomycin (from the 1st day to the 5th day of hospitalization) and fluconazol (single dose on the 3nd day of hospitalization), as well as three days of cefuroxime (Zinnat®) prior to admission.).
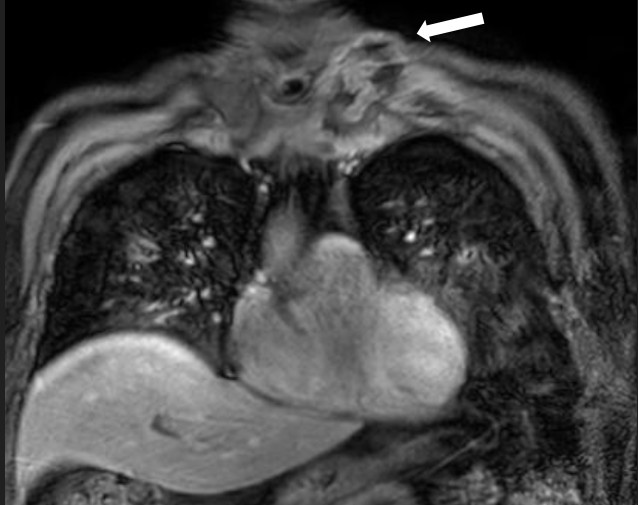
Figure 2. Sagittal magnetic resonance imaging (POS-DIXON) (Multi-Dixon). Lytic lesion with ill-defined contour and soft tissue edema (stenoclavicular)
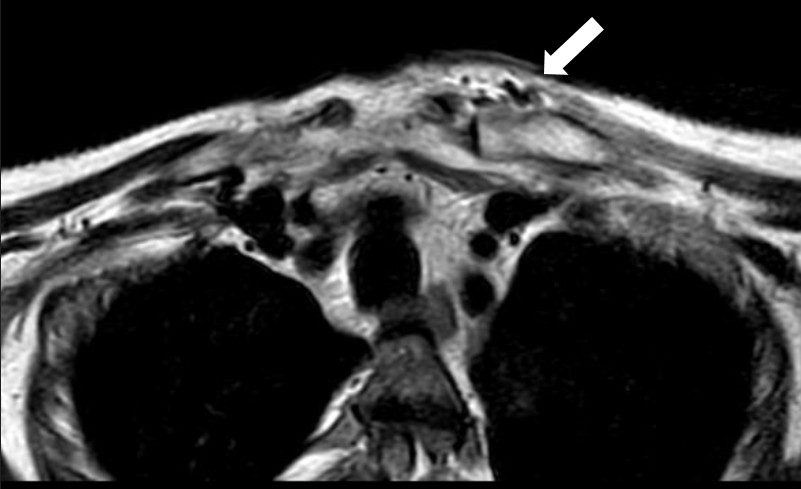
Figure 3. Axial magnetic resonance imaging. Lytic lesion with periosteal reaction characteristic of osteomyelitis.
After confirming MSSA, IV cefazolin was initiated for a planned 14-day course, following four days of oxacillin (from the 5th day to the 9th day of hospitalization.
Therapeutic management included thromboprophylaxis with enoxaparin, gastric protection with pantoprazole, nutritional support, physical therapy, speech therapy, and glycemic control using NPH insulin (17 IU in the morning and 6 IU at night), as HbA1c was recorded at 13.5% on October 24. The patient also received clonazepam for agitation. The patient showed good clinical progress, with regression of the infection, absence of pain (VAS = 0), hemodynamic stability, and improvement in laboratory parameters.
Other procedures included negative veneral disease research laboratory (VDRL) , pending cytomegalovirus, and use of topical ketoconazole for the treatment of balanoposthitis. The vascular and thoracic surgery teams recommended continuation of conservative treatment with antibiotics, with no need for further surgical intervention.
Within 20 days of admission, the medical team reviewed the therapeutic plan and opted for a transition to oral cefuroxime following completion of the intravenous course. The oral regimen was scheduled to complete a total of 8 weeks of antimicrobial therapy, subject to clinical and laboratory reassessment..

Figure 4. Coronal magnetic resonance imaging ESAG T2. Osteolytic lesion in sternal profile with periosteal reaction of the manubrio.
Hospital discharge was planned for the following days, provided the therapeutic response remained favorable.
The patient remained under outpatient care, with normal inflammatory and infectious parameters. Clinically, a scar was observed without inflammatory signs, and his diabetes and hypertension remained well controlled. In April 2025, he sought medical attention for a urinary tract infection and was hospitalized for treatment. This condition was unrelated to the previously treated osteomyelitis, from which only a dry scar remained, without pain or bulging.
Discussion
The sternoclavicular joint is a structure that connects the breastbone (sternum) to the clavicle, and plays a crucial role in stabilizing and enabling movements of the shoulder girdle, allowing a wide range of shoulder mobility (7). Infections in the sternoclavicular joint warrant prompt attention due to their proximity to vital structures such as the subclavian vessels and the phrenic nerve. If not treated swiftly, such infections can spread and cause serious damage to these critical anatomical regions (8).
Sternoclavicular septic arthritis is a rare infection that requires complex treatment due to its proximity to important vascular structures. Staphylococcus aureus is the most common causative agent, both in healthy adults and in those with risk factors such as diabetes, intravenous drug use, or chronic renal failure (9). A study observed a predominance of sternoclavicular septic arthritis in men with diabetes, intravenous drug use, trauma, smoking, and immunosuppression. The most common complication was clavicular osteomyelitis (64% of cases) (10). Septic arthritis of the sternoclavicular joint presents unilaterally in 95% of cases. However, it can occur bilaterally, usually as a secondary manifestation of infective endocarditis (11).
Osteomyelitis is an infection that affects bone tissue and can occur in various anatomical locations. After the vertebrae, the most common sites of hematogenous osteomyelitis are the flat bones of the axial skeleton, such as the sternoclavicular joint and the pelvis (7). While osteomyelitis is an infection of the bone (7), arthritis is an inflammation or infection of the joint (11).
Acute hematogenous osteomyelitis is a bone infection caused by the spread of bacteria through the bloodstream, which then settle and proliferate within bone tissue (12). Bacterial invasion tends to occur more readily in vulnerable individuals, such as postoperative patients or those with open injuries (13).
The incidence of bacterial osteomyelitis is estimated at 92 cases per 100,000 adults, with hematogenous osteomyelitis affecting more frequently children and the elderly (14). Diabetic patients have a high rate of persistent colonization with Staphylococcus aureus, which increases the risk of hospitalization for serious infections. Poorly controlled diabetes mellitus, combined with complications such as neuropathy and chronic wounds, creates a favorable environment for colonization to progress to serious infections (15).
In the present case, methicillin-sensitive Staphylococcus aureus was isolated - the most commonly identified pathogen in osteomyelitis, as reported in the literature. Hematogenous osteomyelitis is usually monomicrobial, although in intravenous drug users, it may also involve Pseudomonas aeruginosa or Serratia marcescens (16).
The main risk factors include intravenous drug use, diabetes mellitus, and obesity and patients typically present with local pain and swelling, often accompanied by systemic symptoms (1).
Osteomyelitis is caused by bacteria capable of forming biofilms, making treatment more challenging. The process involves infection, bone necrosis, and the formation of sequestra. Symptoms are non-specific (pain, fever, and swelling) requiring laboratory and imaging studies to establish a definitive diagnosis (13).
In this case, the elderly patient presented with progressive shoulder pain migrating to the anterior thoracic region, associated with a painful nodule in the sternal notch. He also experienced persistent fever, significant weight loss, and difficulty sleeping and breathing while lying down. On admission, he reported localized pain, though swelling was not evident.
Initially, his condition was thought to be cellulitis, considered an early or superficial manifestation of a deeper infectious process, which later progressed to a confirmed diagnosis of osteomyelitis. The patient had notable comorbidities, including uncontrolled type 2 diabetes mellitus and systemic arterial hypertension. Because primary infection of the sternoclavicular joint occurs without a nearby infectious focus, it is usually attributed to hematogenous spread from another site (1).
Osteomyelitis should be suspected in patients presenting with musculoskeletal pain and systemic symptoms such as fever and malaise, especially when risk factors like poorly controlled diabetes, chronic wounds, neuropathy or intravenous drug use are present. On physical examination, findings may include erythema, bone tenderness, and restricted movement, and differential diagnoses include soft tissue infections, gout, fractures, Charcot arthropathy, and other conditions. Workup involves laboratory tests (complete blood count, CRP, ESR, blood cultures) and imaging studies – with plain radiography and, especially, magnetic resonance imaging (which is more sensitive). Confirmation is achieved through bone biopsy culture, considered the gold standard, though not always required when blood cultures and imaging are sufficiently diagnostic (16).
People with chronic illnesses, such as diabetes or renal failure, and smokers are at higher risk of bacterial osteomyelitis. In diabetic patients, the infection more often involves the feet, particularly in the presence of ulcers (14). However, in some cases, even individuals without obvious risk factors may develop osteomyelitis, which reinforces the importance of a thorough clinical investigation when chest pain of unclear origin persists (3).
Umair, Farooq and Maka (7) described a case involving an 85-year-old patient with comorbidities such as diabetes, hypertension, and ischemic heart disease, who developed sternoclavicular infection with rapid progression to sepsis and death. In comparison, the 64-year-old patient presented here also had diabetes and hypertension, with symptoms of chest pain, fever, and weight loss, which ultimately progressed to hematogenous sternoclavicular osteomyelitis. Both cases involved the sternoclavicular joint and significant comorbidities. And both patients underwent multidisciplinary evaluation, imaging and laboratory testing, and intravenous antibiotic therapy. The main difference lies in the outcome: the patient described by Umair, Farooq and Maka (7) succumbed to the infection, while the present patient responded well to treatment and was anticipated to be discharged.
Al Ahmari and Alanis (17) reported the case of a 66-year-old diabetic patient with right shoulder pain, fever, and muscle limitation, rapidly progressing to sepsis. Imaging confirmed sternoclavicular septic arthritis with extensive abscess and clavicular osteomyelitis caused by Staphylococcus aureus. Treatment included initial emergency debridement followed by further surgery to control persistent wound secretion, supplemented by antibiotic therapy (4 weeks of IV cloxacillin, 2 weeks of IV cefazolin, and 2 weeks of oral cefuroxime). While in the report by Al Ahmari and Alanis (17), the patient required reoperation due to persistent secretion, this case was resolved with a single surgical drainage. Both patients underwent 8 weeks of antibiotic therapy, but in this report, a more intensive initial regimen (piperacillin/tazobactam + vancomycin) was used before adapting to IV cefazolin (14 days) and oral cefuroxime.
Furthermore, in the present case, the patient had decompensated diabetes (HbA1c 13.5%), but improved, perhaps due to early surgical intervention and, associated with the initial broad antibiotic coverage
Osteomyelitis treatment requires an integrated approach, usually antibiotics, and, in many cases, surgical intervention, depending on the stage of disease and overall patient condition. Antibiotic selection should ideally be guided by culture results, but in severe cases, such as sepsis or neurologic compromise, empirical therapy may be initiated earlier (16). Often, antibiotics alone are insufficient, and surgical debridement becomes necessary to remove infected or necrotic tissue (2), which may be supplemented with bone stabilization and the use of antibiotic-impregnated sponges (16).
This case report has inherent limitations, characteristic of descriptive studies, particularly the lack of long-term follow-up. The patient’s clinical course was monitored only during hospitalization, which limits our ability to assess long-term therapeutic success or outpatient outcomes.
Despite limitations, the case contributes to the literature by documenting a rare instance of hematogenous sternoclavicular osteomyelitis in an elderly patient with uncontrolled diabetes and hypertension. The case underscores the importance of clinical suspicion in patients with nonspecific symptoms like anterior chest pain and weight loss, and emphasizes the need for a comprehensive diagnostic approach using sensitive laboratory and imaging techniques. This case highlights the value of a multidisciplinary approach, including medical management, nutritional support, physical therapy, and tight control of comorbidities, in achieving a favorable therapeutic outcome.
Take home message: The main lessons learned from this case report include the importance of considering differential diagnoses beyond common musculoskeletal conditions, such as bursitis, when faced with persistent pain associated with systemic signs and weight loss. This case highlights that sternoclavicular osteomyelitis can occur through hematogenous spread, especially in patients with comorbidities such as decompensated diabetes mellitus, which reinforces the need for detailed clinical and laboratory investigations, microbiological analysis, and imaging. The importance of a multidisciplinary approach, culture-guided antimicrobial therapy, early intervention, and metabolic control for a positive outcome is emphasized. The combination of early diagnosis, targeted therapy, and appropriate support is essential for successful treatment.
Conclusion
Although rare, sternoclavicular osteomyelitis is a serious condition that requires heightened clinical awareness due to its nonspecific presentation. Symptoms such as chest or shoulder pain, fever, and weight loss may be misattributed to other pathologies, delaying diagnosis. This case emphasizes the critical role of imaging and laboratory tests in the early detection of bone and joint infections, enabling a more accurate diagnosis. Treatment with targeted antibiotic therapy, combined with clinical support measures, led to the resolution of the infection and prevented more severe systemic complications.
Clinical examination remains essential for early identification of signs suggestive of osteoarticular infections. In the case presented, a careful clinical assessment raised suspicion for a condition beyond simple bursitis, leading to appropriate diagnostic testing that confirmed sternoclavicular osteomyelitis. Thus, attentive clinical listening, detailed physical examination, and correlation with patient history remain indispensable tools in medical practice, particularly when dealing with broad differential diagnoses and nonspecific presentations.
Ethics: Written informed consent was obtained from patient for all procedures and for the publication of this case report.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: Conceptualization: N.G.A. Investigation: N.G.A, L.P.L.C.O., O.S.S., B.C.Z. and C.M.A.L.R. Methodology: N.G.A. and B.C.Z. Validation: N.G.A. and B.C.Z. Visualization: J.R.B., B.K.C.P. and N.G.A. Writing – original draft: N.G.A. Writing – review & editing: N.G.A., O.S.S. and B.C.Z. Supervision: O.S..S and BCZ. All authors approved final version for publication and fulfilled authorship criteria.
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: Authors did not use AI-assisted technologies in preparation of this manuscript
Data and material availability: Does not apply
References
| 1. Ali B, Shetty A, Qeadan F, Demas C, Schwartz JD. Sternoclavicular joint infections: Improved outcomes with myocutaneous flaps. Semin Thorac Cardiovasc Surg 2020; 32: 369-76. doi: 10.1053/j.semtcvs.2019.12.007 https://doi.org/10.1053/j.semtcvs.2019.12.007 PMid:31866574 |
||||
| 2. Al Ani A, Abdelmonem K, Forsat K, Alqaderi N, Teir H. Primary sternal osteomyelitis: A case report. Int J Surg Case Rep 2023; 110: 108654. Doi: 10.1016/j.ijscr.2023.108654 https://doi.org/10.1016/j.ijscr.2023.108654 PMid:37591189 PMCid:PMC10457543 |
||||
| 3. Jaheddin F, Messaoud O, El Aoufir O, Jroundi L. Primary sternal osteomyelitis in an immunocompetent adolescent. Radiol Case Rep 2025; 20: 2829-32. Doi: 10.1016/j.radcr.2025.02.070 https://doi.org/10.1016/j.radcr.2025.02.070 PMid:40176977 PMCid:PMC11964591 |
||||
| 4. Baraboutis IG, Argyropoulou A, Papastamopoulos V, Psaroudaki Z, Paniara O, Skoutelis AT. Primary sternal osteomyelitis caused by Nocardia nova: case report and literature review. Braz J of Infect Dis 2008; 12: 257-9. Doi: 10.1590/S1413-86702008000300018 https://doi.org/10.1590/S1413-86702008000300018 PMid:18833413 |
||||
| 5. Lopez Christopher DBA, Hill JBMD, Stavropoulos CMD, Lerman OZMD. Primary sternal osteomyelitis: A case Report and review. Plastic Reconstr Surg - Global Open 2019; 7: e2120. doi: 10.1097/GOX.0000000000002120 https://doi.org/10.1097/GOX.0000000000002120 PMid:31624660 PMCid:PMC6635211 |
||||
| 6. Shukla PC. Primary sternal osteomyelitis. J Emerg Med 1994; 12: 293-7. https://doi.org/10.1016/0736-4679(94)90269-0 PMid:8040584 |
||||
| 7. Umair M, Farooq MU, Maka TA. Multidisciplinary strategies for early diagnosis and treatment of sternoclavicular joint infection: Enhancing outcomes and reducing mortality. Life Sci 2025; 6: 05-05. doi: http://doi.org/10.37185/LnS.1.1.553 https://doi.org/10.37185/LnS.1.1.553 |
||||
| 8. Tasnim S, Shirafkan A, Okereke I. Diagnosis and management of sternoclavicular joint infections: a literature review. J Thorac Dis 2020; 12: 4418-26. doi: 10.21037/jtd-20-761 https://doi.org/10.21037/jtd-20-761 PMid:32944355 PMCid:PMC7475584 |
||||
| 9. Jang YR, Kim T, Kim MC, Sup Sung H, Kim MN, Kim MJ, et al. Sternoclavicular septic arthritis caused by Staphylococcus aureus: excellent results from medical treatment and limited surgery. Infect Dis 2019 ;51: 694-700. doi: 10.1080/23744235.2019.1639810 https://doi.org/10.1080/23744235.2019.1639810 PMid:31355687 |
||||
| 10. Bayfield NGR, Wang E, Larbalestier R. Medical and conservative surgical management of bacterial sternoclavicular joint septic arthritis: a case series. ANZ J Surg 2020; 90: 1754-9. doi: 10.1111/ans.16019 https://doi.org/10.1111/ans.16019 PMid:32483916 |
||||
| 11. Masmoudi K, Elleuch E, Akrout R, Feki A, Ezzeddine M, Fourati H, et al. Bilateral septic arthritis of the sternoclavicular joint complicating infective endocarditis: a case report. J Med Case Rep 2018; 12: 205. doi: 10.1186/s13256-018-1709-9 https://doi.org/10.1186/s13256-018-1709-9 PMid:29973288 PMCid:PMC6033282 |
||||
| 12. Cunha LAM, Oliveira Filho OBA, Ohara G, Skaf AY. Osteomielite hematogênica aguda. Sociedade Brasileira de Ortopedia e Traumatologia, Associação Brasileira de Cirurgia da Mão, Colégio Brasileiro de Radiologia; 2007. | ||||
| 13. Pedro MCS, dos Santos Marques JV, de Arruda ITS. Mecanismos patológicos da osteomielite aguda provocada por infecções oportunistas. Braz J Health Rev 2025; 8: e79209-e79209. https://doi.org/10.34119/bjhrv8n2-351 |
||||
| 14. Costa, NS, Batista RF, Nascimento GS, Cantanhede R. Osteomielite bacteriana aguda e crônica no pós-trauma de membros inferiores em adultos. Revista ft: ciências da saúde 2023; 1-40. | ||||
| 15. Hart J, Hamilton EJ, Makepeace A, Davis WA, Latkovic E, Lim EM, et al. Prevalence, risk factors and sequelae of Staphylococcus aureus carriage in diabetes: the Fremantle Diabetes Study Phase II. J Diabet Compl 2015; 29: 1092-7. doi: 10.1016/j.jdiacomp.2015.06.005 https://doi.org/10.1016/j.jdiacomp.2015.06.005 PMid:26243688 |
||||
| 16. Bury DC, Rogers TS, Dickman MM. Osteomyelitis: Diagnosis and Treatment. Am Fam Physician 2021; 104: 395-402. | ||||
| 17. Al Ahmari AM, Alanis IM. Sternoclavicular joint septic arthritis and osteomyelitis. J. Musculoskelet Surg Res 2019; 3: 363. doi: 10.4103/jmsr.jmsr_25_19 https://doi.org/10.4103/jmsr.jmsr_25_19 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

