Anomalous origin of right coronary artery from left coronary sinus associated with aneurysm of aortic root
CASE REPORT
Anomalous origin of right coronary artery from left coronary sinus associated with aneurysm of aortic root
Article Summary
- DOI: 10.24969/hvt.2018.80
- Page(s): 123-129
- Cardiac Surgery
- Published: 28/09/2018
- Received: 12/09/2018
- Accepted: 28/09/2018
- Views: 11158
- Downloads: 8467
-
Citations
- Keywords: anomalous origin, coronary artery, sudden cardiac death, aneurysm of aortic root, David I operation
PDF PRINT VERSION CommentsAddress for CorrespondenceKuat B.Abzaliyev, AN Syzganov National Scientific Center of Surgery, Almaty, Kazakhstan
Email: abzaliev_kuat@mail.ru
Authors
Rustem M. Tuleutayev, Daurenbek O. Urazbekov, Kuat B. Abzaliyev, Kyanysh O. Ongarbayev
AN Syzganov National Scientific Center of Surgery, Almaty, Kazakhstan
Abstract
Prevalence of anomalous origin of right coronary artery (RCA) from left coronary sinus in population according to autopsy studies is 0.026%. Origin of left main coronary artery and RCA from opposite sinus of Valsalva with further course of anomalous vessels between aorta and pulmonary artery often is linked to sudden death. We present a case of anomalous origin of RCA from left coronary sinus and aneurysm of aortic root. Our case demonstrates that when both coronary arteries` ostia are close to each other coronary arteries can be re-implanted on common area. Firstly, this prevents distention and deformation of coronary arteries that might cause myocardial infarction. Secondly, it reduces time of placing anastomosis thus decreasing period of myocardial ischemia and cardiopulmonary bypass time.
Introduction
Anomalous origin of right coronary artery (RCA) – a rare congenital anomaly, was for the first time described by White and Edwards (1). According to autopsy studies, prevalence of this anomaly in Caucasians is 0.026% (2). However, its prevalence in other populations is significantly higher. Kaku et al. (3) in their study of 17731 patients undergoing coronary angiography in Japanese centers between 1968 and 1994 observed prevalence of anomalous origin of coronary artery to be 0.25%. Topaz et al. (4), reported similar results and noticed that anomalous origin of RCA is the most prevalent coronary anomaly in Hispanic population.
In most cases, coronary artery anomalies are not detected clinically because either they do not manifest by symptoms or the sudden death is the first and last sign of the disease. Less than 30% of adult population has symptoms before the establishing diagnosis of coronary artery anomaly. More often anomaly of coronary artery is a random finding during imaging study, coronary angiography and autopsy. The certain forms of anomalies are associated with the risk of sudden death and myocardial ischemia. Origin of left main coronary artery and RCA from opposite sinus of Valsalva with further course of anomalous vessels between aorta and pulmonary artery trunk often is linked to sudden death. Specifically, this anomaly is characterized by aberrant coronary artery with split ostium and course in proximal part with obtuse angle. In such kind of anomaly, the artery during physical exertion distends with impairment of blood supply through narrow origin. Increase in stroke volume during physical exertion is related to stretching of aorta and pulmonary trunk, which also contributes to blood flow reduction in anomalous artery (5).
The aim of our case report is to describe rare anomaly of coronary artery origin concomitant with aortic root aneurysm, as well as to present the results of surgical correction of this pathology.
Case
A 61-year-old patient on 23.02.2018 was admitted to cardiac surgery department of AN Syzganov NNCS with complaints on periodic burning chest pain spreading to the left arm, overall weakness, rapid fatigue, and periodic headache.
Diagnosis of coronary artery disease had been established 2 months before hospitalization when due to sharp chest pain of burning character and dyspnea, the patient called ambulance. He was hospitalized to the Almaty hospital with diagnosis of acute coronary syndrome without ST elevation. He received aspirin 325 mg, heparin 5000 U iv and nitrates infusion on pre-hospital stage in ambulance. He was hospitalized to the roentgeno-surgical department of the hospital. On admission his chest pain relieved and he was scheduled to coronary angiography. Diagnosis of left ventricular anterior wall non-ST-elevation myocardial infarction was established. He received treatment. At the same hospital the aneurysm of ascending aorta was diagnosed on echocardiography and after consultation of cardiac surgeon from AN Syzganov NNCS he was scheduled for cardiac surgery.
On admission: Electrocardiogram (ECG) (Fig. 1) revealed sinus bradycardia 55 beats per minute, PQ-0.2 s, QRS -0.09s, QRST-0.38 s, left ventricular hypertrophy, myocardial scar changes.
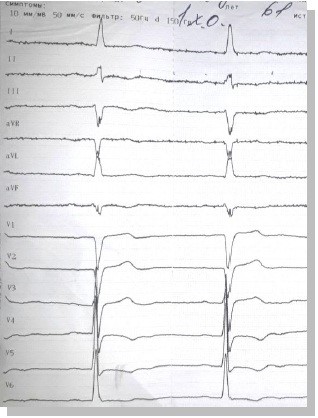
Figure 1. Preoperative electrocardiogram
Echocardiography (echo) (Fig. 2): Aortic valve (AV) fibrous ring 2.6 cm, regurgitation 2cm. Mitral valve (MV), regurgitation 1 cm. Tricuspid (TV) and pulmonary (PV) valves are normal. Diameter of aorta ascending part - 4.1 cm, arch – 3.3 cm, aortic sinus 5.6 cm, descending part 2.9 cm. Left atrial (LA) size – 2.4 cm, left ventricular end-diastolic diameter (LVEDD) 6.7 cm, end-systolic diameter (LVESD) 4.5 cm, end-diastolic volume (EDV)-234 ml, end-systolic volume (ESV) 73 ml, stroke volume (SV) 161 ml, ejection fraction (EF) – 68%. Interventricular septal thickness (IVST) -1.5 cm, left ventricular posterior wall thickness (LVPWT) 1.3 cm, right ventricular systolic pressure 30 mmHg.

Figure 2. Dilatation of sinus of Valsalva 56 mm, aortic regurgitation 2 cm
Coronary angiography and aortography (28.12.2017)(Fig. 3): Multipositional selective left and right coronary angiography revealed balanced type of coronary circulation. Left main coronary artery stem brief and patent, left anterior descending artery –patent through all its length, 1st diagonal branch of enlarged caliber and patent through entire length. Circumflex, RCA and their branches are patent through entire length. Selective angiography of common carotid arteries: left common carotid artery, external carotid artery – with smooth contour and patent, internal carotid artery – kinking at mid-portion. Right common carotid artery and external carotid artery – with smooth contour and patent, internal carotid artery – kinking at proximal part.
Contrast enhanced multidetector computed tomography (MDCT) 29.12.2017 (Fig. 4). Aneurysmatic dilatation of aortic root 56 mm. Anomalous origin of RCA from left coronary sinus.
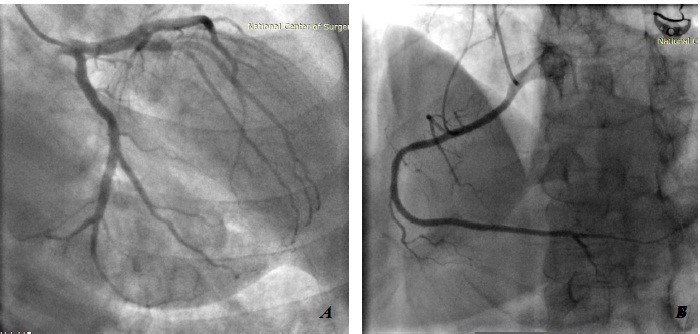
Figure 3. Coronary angiography and angiography of aortic arch: A – left coronary artery B – RCA
RCA- right coronary artery
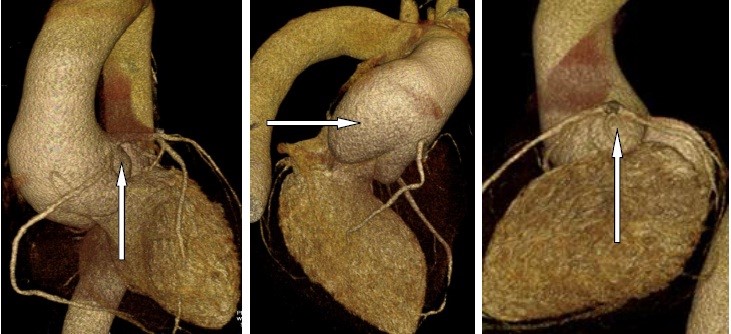
Figure 4. Contrast enhanced multidetector computed tomography. Aneurysmatic dilatation of aortic root 56 mm. Anomalous origin of RCA from left coronary sinus.
RCA- right coronary artery
Taking in account clinical and ECG, echocardiographic, angiography and contrast-enhanced MDCT data, patients underwent surgery: re-implantation of aortic valve –David I procedure under cardiopulmonary bypass, moderate hypothermia and pharmacological and cold cardioplegia (Fig. 5). Intraoperatively: there was marked dilatation of aortic root (Fig. 5A); anomalous origin of RCA from left coronary sinus was confirmed (Fig. 5B); aortic valve was re-implanted in the vascular prosthesis N30, coaptation of aortic valve cusps was satisfactory (Fig. 5C). Coronary arteries ostia were re-implanted in unified block in in prosthesis in the left coronary sinus area (Fig.5D and 5E). Distal anastomosis was performed in the non-dilated part of aorta (Fig. 5F).
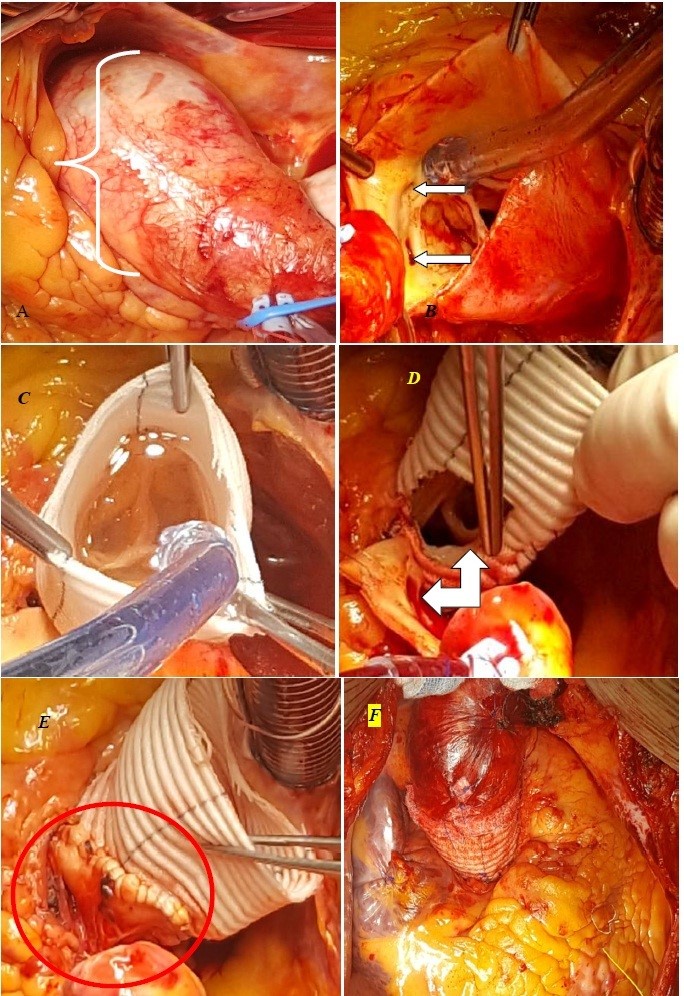
Figure 5. David I re-implantation of aortic valve: A – aneurysm of aortic root and ascending aorta part. B – an arrow points at anomalous origin of right coronary artery from left coronary sinus, C- re-implantation of aortic valve into vascular prosthesis N30, coaptation of aortic valve cusps is satisfactory D Coronary arteries` ostia are re-implanted in unified block manner in prosthesis in left coronary sinus view, F – the complete view.
Postoperative period was unremarkable (Fig. 6). ECG – sinus rhythm 65 bpm. Echo – there is no aortic regurgitation, mean gradient is 5 mmHg. LVEDD -6.0 cm, LVESV -4.0 cm. Patient was discharged on the 6th day after surgery in satisfactory condition for the follow-up by cardiologist.Follow-up examination one month after surgery: Echo (28.03.2018) – AV – maximal gradient 5 mmHg. Mean gradient 3 mmHg. Aortic cusps are thin and mobile. MV – E/a 0.8. Leaflets are thickened and mobile. PV – cusps are thin and mobile. TV leaflets thin and mobile. Ascending aorta diameter 3.4 cm, aortic arch diameter 2.9 cm. Aortic sinus -3.2 cm, descending aorta-2.4 cm. LA – 3.4 cm, LVEDD-5.5.cm, LVESD -3.6 cm, LVEDV-152 ml, LVESV – 56 ml, SV – 96 ml, EF 62%. IVST – 1.3 cm, LVPWT -1.0 cm. RV systolic pressue 27 mmHg. LV contractility satisfactory. Pericardium: small amount of fluid. Conclusion: Heart after surgery condition. LV diastolic dysfunction type 1. LV hypertrophy (IVST).
ECG one month follow-up (28.03.2018) (Fig. 7). Sinus rhythm, regular, 67 bpm. PQ-0.26 s, QRS -0.26 s, QRST 0.32 s, RR-90 s. Left axis deviation. LV hypertrophy.
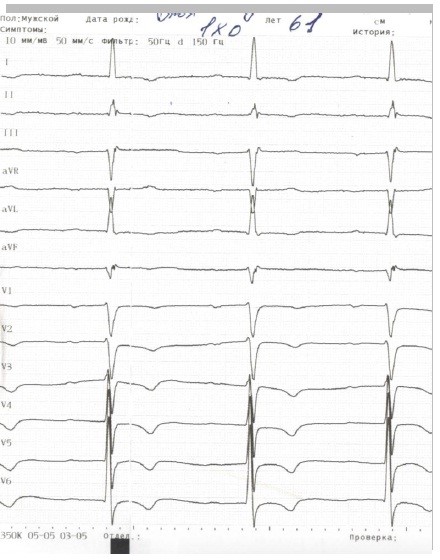
Fig 6. – ECG in early postoperative period
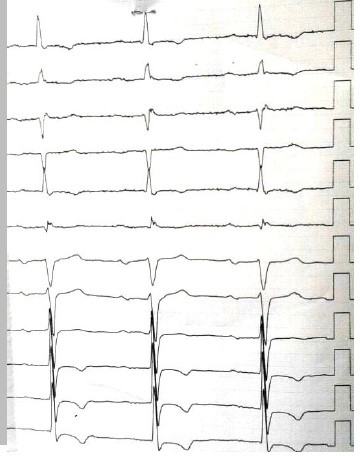
Fig 7. Follow-up ECG one month after surgery
Discussion
One registry study reported that among 387 sudden deaths among young athletes, 53 (13.7%) were due to coronary anomalies, with majority of anomalous origin from opposite coronary sinus.
When patients with anomalous coronary artery complain on chest pain or dyspnea, it must arise suspicion on condition that might lead to sudden death (6). In our case, physician missed anomalous origin of coronary artery during selective coronary angiography. Computed tomography in cardiac vascular mode is an appropriate method for diagnosis of anomalous coronary arteries and it was performed next day after coronary angiography. Specifically, computed tomography with 64 and higher detectors are capable of imaging correctly pathology of coronary arteries with precision as selective coronary angiography (7). Then analyzing MDCT image we discovered anomalous origin of RCA. In cases when ECG monitoring was performed in patients with coronary artery anomalies and they die during monitoring the cause of death was ventricular fibrillation (5).
Stress testing also can be useful for objective demonstration of myocardial ischemia. We consider that during increase in exercise load the angle increases facilitating myocardial ischemia. This was demonstrated by Barbie et al. (7).
Choice of treatment of this coronary anomaly is disputable with some opinions to perform revascularization in all cases. Though coronary bypass surgery (CABG) is a routine type of surgery, it has its own disadvantages. It is known that in young patients with potential long life expectancy, venous grafts are no preferable because of limited long-term patency of the vein. Arterial grafts are not suitable for this kind of surgery and case, because they tend to atrophy and are not developing because of concurred coronary flow, when they are being used for CABG in cases of insignificant stenosis of coronary arteries.
Di Lello et al (9) suggested that translocation RCA to the respective sinus is suitable type of surgery. Rinaldi et al. proposed removal of common wall between RCA and aorta (10). Wolf et al. (11) in a patient with anomalous origin of left coronary artery performed anatomical correction creating neo-ostium and separating 2 ostia for left and right coronary arteries, and in addition made the left internal mammarian artery to left anterior descending artery graft. Stenting of anomalous RCA may be very technically difficult with unclear long-term success and is being used only in few centers. In Japan, there is a more conservative approach. Kaku et al (3) included in their study 56 patients with anomalous origin of coronary arteries and treated them with beta-blockers. In their study, patients had low blood pressure and arrhythmias on exertion; however, 5-year mortality was not due to congenital coronary anomaly (3).
In our patient aneurysm of aortic root >5.5 cm and aortic regurgitation +2 were revealed that itself is indication for surgery. Intraoperatively anomalous origin of RCA from left coronary sinus was confirmed. Due to close position of both coronary arteries` ostia, preserved aortic valve and aneurysm of aortic root we performed reimplantation of aortic valve by David I with reimplantation of coronary arteries` ostia on common ground on left neosinus. The good coaptation of aortic valve cusps was reached. There were no stretching and deformation of coronary arteries. This tactics was proven true and we reached an excellent result.
Conclusions
In our case, aneurysm of aortic root and dilatation of sinus of Valsalva produced additional traction and compression of anomalously located RCA. This stimulated development of acute coronary syndrome, which was successfully treated on pre-hospital state.
This case shows that when ostia of both coronary arteries are closely located it is possible to re-implant coronary arteries on common ground. Firstly, this prevents deformation of coronary arteries that can cause myocardial infarction. Secondly, it reduces time of placing anastomosis, decreases myocardial ischemia time and cardiopulmonary bypass time.
Peer-review: Internal and external
Conflict of interest: None to declare
Authorship: R.M.T., D.O. U., K.B.A., K.O.O. equally contributed to management of case and preparation of case report.
Acknowledgement and funding: None to declare
Ethics: Informed consent was obtained from patient for all procedures
References
1.White NK, Edwards JE. Anomalies of the coronary arteries. Report of four cases. Arch Pathol 1948; 45: 766-71. 2.Alexander RW, Griffiths GC. Anomalies of the coronary arteries and their clinical significance. Circulation 1956; 14: 800-5. https://doi.org/10.1161/01.CIR.14.5.800 3.Kaku B, Shimizu M, Yoshio H, Ino H, Mizuno S, KanayaH, et al. Clinical features of prognosis of Japanese patients with anomalous origin of the coronary artery. Jpn Circ J 1996; 60: 731-41. https://doi.org/10.1253/jcj.60.731 PMid:8933235 4.Topaz O, DeMarchena EJ, Perin E, Sommer LS, Mallon SM, Chahine RA. Anomalous coronary arteries: angiographic findings in 80 patients. Int J Cardiol 1992; 34: 129-38. https://doi.org/10.1016/0167-5273(92)90148-V 5. Tseluyko VI, Mishuk NE, Kinoshenko KYU. Anomalies of coronary arteries (part 1). Liki Ukraini razdel diabet serdtse 2012; 10: 166. 6.Angelini P. Coronary artery anomalies-current clinical issues: definitions, classification, incidence, clinical relevance, and treatment guidelines. Tex Heart Inst J 2002; 29: 271-8. PMid:12484611 PMCid:PMC140289 7.Berbarie RF, Dockery WD, Johnson KB, Rosenthal RL, Stoler RC,Schussler JM. Use of multi-slice computed tomographic coronary angiography for the diagnosis of anomalous coronary arteries. Am J Cardiol 2006; 98: 402-6.https://doi.org/10.1016/j.amjcard.2006.02.046 PMid:16860032 8.Maron BJ. Sudden death in young athletes. N Engl J Med 2003; 349: 1064-75. https://doi.org/10.1056/NEJMra022783 PMid:12968091 9.Di Lello F, Mnuk JF, Flemma RJ, Mullen DC. Successful coronary reimplantation for anomalous origin of the right coronary artery from the left sinus of Valsalva. J Thorac Cardiovasc Surg 1991; 102: 455-6. PMid:1881185 10.Rinaldi RG, Carballido J, Giles R, Del Toro E, Porro R. Right coronary artery with anomalous origin and split ostium. Ann Thorac Surg 1994; 58: 829-32 https://doi.org/10.1016/0003-4975(94)90760-9 11. Wolf T, Bolotin G, Ammar R, Uretzky G. Anomalous origin of the left main coronary artery: anatomical correction and concomitant LIMA-to-LAD grafting. Eur J Cardiothorac Surg 1999; 15: 209-12. https://doi.org/10.1016/S1010-7940(98)00307-8 Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.Archive of Issues
AUTHOR'S CORNER
 Authors having problems with submissions please notify editor: editor@hvt-journal.com
Authors having problems with submissions please notify editor: editor@hvt-journal.com
