Experience in laparoscopic cholecystectomy in Nobel Medical College, Nepal
ORIGINAL RESEARCH ARTICLE
Experience in laparoscopic cholecystectomy in Nobel Medical College, Nepal
Article Summary
- DOI: 10.24969/hvt.2018.82
- Page(s): 11-15
- General Surgery
- Published: 24/02/2019
- Received: 20/09/2018
- Revised: 05/10/2018
- Accepted: 05/12/2018
- Views: 11086
- Downloads: 8068
- Keywords: cholecystectomy, laparoscopy, elective, conversion, complications, mortality, gallstone, cholecystitis
Address for correspondence: Ruslan Sulaimankulov, Department of General Surgery, Nobel Medical College Teaching Hospital, Kanchanbari, Biratnagar-5,
Nepal, Mobile: +977 9802330898, +977 9842330898, Email: ruslansulaimankulov@gmail.com
Ruslan Sulaimankulov, Chittaranjan Das*, Gulmira Jolochieva**, Ashok Koirala, Rupak Bhattarai*
Department of General Surgery, *Department of Anesthesiology, Critical Care & Pain Management, **Department of Obstetrics & Gynecology, Nobel Medical College Teaching Hospital and Research Centre, Biratnagar, Nepal
Abstract
Objective: A laparoscopic cholecystectomy (LC) is the treatment of choice for gallbladder diseases. The aim of this study is to analyze laparoscopic cholecystectomies performed by a single surgeon over 8 years at Nobel Medical College Teaching Hospital and Research Centre Pvt. Ltd. of Biratnagar, Nepal (NMCTH).
Methods: We performed a retrospective analysis of 7557 patients that underwent a LC by a single surgeon, from October 2010 to July 2018. We divided it into 3 groups that include data of every three years.
Results: The hospital stay, operation time and conversion rates were decreased by years of experience. Female patients outnumbered male (M:F=1:3.7) patients in this study. The hospital stay (3 days), operation time (21 min), conversion (0.3%) and complications (1.9%) rates decreased from Group 1 to Group 3 (p<0.05).
Conclusion: As surgical experience increased with a rising number of cases, the conversion rate, complications, hospital stay and mean operation time decreased.
Key words: cholecystectomy, laparoscopy, elective, conversion, complications, mortality, gallstone, cholecystitis
Introduction
Archaeologists have found gallstones in the body of a young woman who lived as early as 2000 years ago. Nowadays, cholecystectomies are occupying the top of operating lists of any hospital in the world (1, 2). About 10-20% of adult population are diagnosed with gallstones (3). The 1st successful cholecystectomy was performed by Langenbuch in 1882 (4). Since the performance of the 1st laparoscopic cholecystectomy (LC) by Prof. Dr. Med Erich Muhe of Boblengen, Germany in 1985, and later by Phillip Mouret in France, LC has become the standard treatment approach (5-8).
Currently almost all cholecystectomies (about 90-93%) in developed countries are performed through laparoscopic surgery (9). LC is considered the gold standard for surgical treatment of gallstone diseases - it causes less pain, better cosmetic effect, which leads to shorter hospital stay and less disability (10).
The factors, which increase the risk for postoperative mortality in LC are old age, co-morbid conditions and acute presentation. Complications can occur in 8-11% of cases (8, 11). Serious complications happen in two major areas: access complications and bile tree injuries. The other complications are very rare, approximately in 0.5% of cases (12). Biliary injury results from poor dissection and failure to adequately define the surgical anatomy (13-15).
The outcome of LC depends on the training, experience and skills of the surgeon (16, 17).
The American College of Surgeons and the Society for Surgery of the Alimentary Tract in their most recent guidelines on the training of laparoscopic surgeons recommended that the surgery is to be performed by a qualified specialist with an appropriate course certificate (18).
The aim of this study is to analyze 7557 cases of LC and observe the changes of outcomes of LC for gallbladder (GB) disease over 8.9 years in our institution.
Methods
Analysis was done retrospectively with the emphasis on the outcome including all complications, conversion rate, hospital stay and operation time after elective cholecystectomy. Cases were selected for inclusion in the study from NMCTH of Biratnagar, Nepal only. Inclusion criteria: the consenting patients of all ages and both sexes with symptomatic cholelithiasis planned for LC. Exclusion criteria: any contraindication to laparoscopic procedure such as pregnancy, bleeding disorder, critical conditions, chronic cardiovascular, pulmonary, liver, kidney diseases; patients having choledocholithiasis, cholangitis, biliary fistula and surgical jaundice.
All patients of all ages and both sexes were studied. Informed written consent was obtained from all the patients who were enrolled in this study and their age and gender were recorded for demographic comparison.
We did retrospective analysis of 7557 cases that underwent a LC performed by a single surgeon, from Kattik 2067 BS (October 2010) to Shrawan 2075 (August 2018). All patients were divided into 3 groups. First group, consisting of 1854 patients, were operated from Kattik 2067 (October 2010) to Kattik 2070 (October 2013), 2nd group - consisting of 3490 patients underwent LC from Kattik 2070 (October 2013) to Kattik 2073 (October 2016) and 2213 patients in the 3rd group had LC from Kattik 2073 (October 2016) to Shrawan 2075 (August 2018).
Preoperatively all patients underwent ultrasonography (USG) to document GB abnormalities. All diagnosed cases of cholelithiasis were prepared for LC. In case of patients with common bile-duct stones identified preoperatively by USG, elective common bile duct (CBD) exploration was planned.
Operative technique
Patients undergoing laparoscopic surgery have been registered prospectively to a database from 2010 to 2018. All patients were operated by standard 4 ports LC.
Cases were taken up for surgery after optimizing investigation parameters and obtaining written consent for operation under general anesthesia. A minimum of 8 hours fasting rule prior to surgery was followed in all cases. Detail pre-anesthetic check up, investigations, preparation and anesthetic techniques were carried out as per hospital protocol. We maintain the vital parameters within limits particularly ETCO2 below 35 mmHg (19).
LC was initiated in all cases with consent for conversion to open surgery or laparoscopic CBD exploration whenever necessary and intraoperative cholangioscopy with stone removal was done.
All patients were monitored closely till discharge and minimum of one postoperative follow up was done in all cases. The average hospital stay was three days. The usual 1st postoperative follow up was in one month after surgery and in case of any complication the patients were readmitted or followed up at regular intervals till full recovery.
Data are presented as number (percentage) and mean values. The outcomes for three groups of patients were compared through a weighted one-way analysis of variance. Weights proportional to the number of cases at each group were used.
Results
Patients
A total of 7557 patients subjected to cholecystectomies includes 5948 female and 1609 male patients (M:F=1:3.7) with a mean age of 41 years. The youngest patient was 6 years old (F) and oldest was 90 years old (F). The most populated age group was 31- 40 years old both among male and female patients. In Group 1 mean age was 39.9 years comparatively in Group 2 and 3 - 40.4 and 41.2 years respectively.
As Figure 1 shows, 79% of patients were females. In Group 1 there were 1479 female, 375 male patients with male and female ratio 1:3,9, Group 2 – 2722 female, 768 male, (M:F=1:3.5), Group 3 – 1747 female, 466 male, (M:F=1:3.7) respectively.
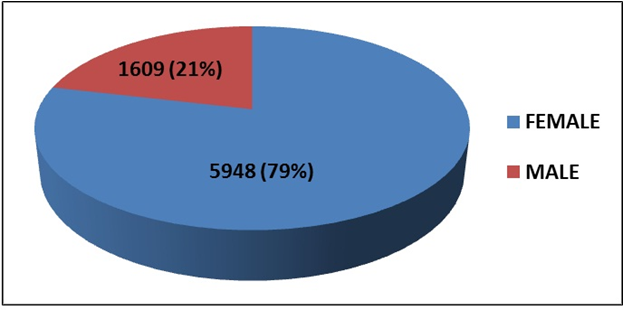
Figure 1. Distribution of patients by sex
Group 1 showed the incidence of GB polyps about 0.8%, in group 2 they were found in 1.8% of cases, and in group 3 their number was significantly high 2.3% (p<0.05).
Overall 5962 patients (78.9%) had symptoms of GB disease – such as jaundice, abdominal pain, and pancreatitis in their anamnesis; 7546 (99.9%) had cholelithiasis, and 11 (0.1%) had acalculous cholecystitis. A total of 6832 patients (90.4%) showed serious anatomical or histological evidence of chronic GB disease and minimal inflammation during the surgery. Other 725 (9.6%) of patients had obvious symptoms of acute cholecystitis. The personal history of 71 patients included jaundice, and 119 of them had suffered pancreatitis in recent or remote past.
Operative findings
Overall 725 patients had acutely inflamed gallbladder; in eight cases there were perforations.
Unexpected common bile-duct (CBD) disease was revealed in 49 patients, including 33 with hepatic duct stones, 8 with biliary obstruction, and 8 with noncalculous cholangitis. Other issues discovered during the surgery included benign GB adenomyomatosis (n=25), cholesterosis (n=8), and cholecystoduodenal fistula (n=16). Eight cases had previously undiscovered cancers, 10 patients had liver cirrhosis and one had chronic hepatitis, and 12 umbilical hernias were repaired during the cholecystectomy.
Common bile-duct/Common hepatic duct stones
Common bile-duct stones were diagnosed preoperatively by USG in 33 patients and were removed in 32 cases by laparoscopic CBD exploration. One patient was referred for ERCP after the gall stones were removed laparoscopically.
Overall, 32 patients had CBD procedures during the LC. Intraoperative cholangioscopy was done in all patients followed by stone removal. In three cases bile-duct stones were pushed into the duodenum, and in all other patients stones were retrieved through CBD incision. In 4 patients bile-duct stones were removed after the laparotomy was converted to open procedure.
A common-duct stone was identified at the time of LC in 1 patient and was removed after the surgery through endoscopic sphincterotomy. In three other cases, small common-duct stones were treated conservatively. Thirty-three patients (0.4%) had common-duct stones identified preoperatively or during the surgery. In 24 other cases stones were removed from the cystic junction and common ducts during the LC.
Outcomes
Conversion from laparoscopic to conventional open cholecystectomy
Out of 7557 patients in the series (Table 1), 22 patients (0.3%) including 8 (0.5%) in Group 1, 9 (0.4%) in Group 2 and 5 (0.3%) in Group 3 had to be converted to conventional cholecystectomy. In 10 cases the conversion was due to inflammatory processes in the GB area. One of the frequent reasons for conversion were adhesions related to previous surgery (two patients); in 4 cases the conversion was due to anomalous anatomical features making dissection difficult or due to mechanical problems with equipment (two cases); The four bile-duct injuries leading to conversion were diagnosed by biliary leakage or dye extravasation during the cholangioscopy. All were repaired during surgery, two with and two without T-tubes. Two of the bowel injuries were at the small intestine, one at the transverse colon, and the another at the duodenum. These bowel injuries were due to the insertion of the trocar without peritoneal visualization. Two more happened under direct visualization at the time of adhesions dissection (Table 1).
|
Table 1. Reasons for conversion from laparoscopic to conventional cholecystectomy |
||||
|
Cause |
Group 1 |
Group 2 |
Group 3 |
Total, n |
|
Inflammation, n |
4 |
4 |
2 |
10 |
|
Adhesions, n |
1 |
1 |
0 |
2 |
|
Bile duct injury, n |
2 |
1 |
1 |
4 |
|
Bowel injuries, n |
1 |
2 |
1 |
4 |
|
Equipment failure, n |
0 |
1 |
1 |
2 |
|
Total, n (%) |
8 (0.5) |
9 (0.4) |
5 (0.3) |
22 (0.3) |
Complications
Overall 185 complications occurred (2.4% of the 7557 patients) in the whole series (Table 2). In 22 (15.6%) due to intraoperative complications, the procedure was converted to open cholecystectomies (Table 1).
The most common postoperative complication was wound infection - 75 (0.99%) patients: 73 patients (32 in Group 1, 23 in Group 2 and 18 in Group 3) had superficial wound infections involving the umbilical trocar insertion site (also gallbladder removal site), and two patients had intraabdominal and liver abscesses that were cured conservatively.
Common hepatic duct injures occurred in 29 (1.6%) patients in Group 1, 28 patients in Group 2 (0.8%) and 12 patients (0.5%) in Group 3, with overall incidence of 0.9% (69 patients). Out of these 69 patients, the injuries of 22 patients were repaired after conversion.
One additional injury developed after conversion to conventional cholecystectomy. Twenty patients with duct injuries were managed laparoscopically. Forty-nine injuries (0.6%) were not recognized until 3, 5, 14 and 24 days after the procedure, till the patients had abdominal distention, abnormal results of liver functional tests or unexplained ileus. Among them 3 patients underwent a second operation by re-laparoscopy (two in Group 1 and one in Group 2) and 7 by re-laparotomy (six in 1 and one in 2), choledochojejunostomy or hepaticojejunostomy were done in these series.
There were 12 intraoperative bleedings (3, 5, 4 respectively in Group 1, 2, 3) and 4 postoperative diagnosed bleedings (1, 2, 1 respectively). One patient with intraoperative uncontrolled bleeding required laparotomy. In two cases, in postoperative period, bleedings were stopped by relaparoscopy and one patient’s bleeding was managed conservatively.
Only four patients in the series had retained common-duct stones, and two patients might have had such stones. These stones were diagnosed after the development of symptoms and abnormal liver functional tests. Endoscopic retrograde cholangiopancreatography showed stones in the two definite cases; in two other cases discovering dilated ducts and indurated papillae suggested the recent passage of stones. There were 41 readmissions (0.5% of all LC): 13 (0.7%) in Group 1, 19 (0.5%) in Group 2 and 9 (0.4%) in Group 3.
One of the common postoperative late complication was incisional (trocar side) hernia which developed from 3 months to 3 years after the surgery. A total of 25 (0.3%) patients were reoperated for herniation (5 (0.3%), 15 (0.4%), 5 (0.2%) respectively for Groups 1, 2, 3).
Two patients (0.03%) died. One patient at first postoperative day had developed necrotizing pancreatitis with uncontrolled vitals. Patient was shifted to intensive care unit, intubated, central venous pressure catheter installed but all therapies were unsuccessful. Second patient had subacute cholecystitis. He had an uncomplicated LC, 1st postoperative day he had acute pulmonary disorders, patient was kept on artificial ventilation, but he died on the 3rd postoperative day.
Overall, complications rate was significantly lower in Group 3 as compared to Groups 1 and 2 (p<0.05) (Table 3).
|
Table 2. Complications of laparoscopic cholecystectomy |
||||
|
Complications |
Group 1 |
Group 2 |
Group 3 |
Total, n(%) |
|
Wound infection total, n superficial, n deep, n |
33 32 1 |
24 23 1 |
18 18 0 |
75 (0.99) 73 2 |
|
CBD injures, n |
29 |
28 |
12 |
69 (0.9) |
|
Bleeding, n |
4 |
7 |
5 |
16 (0.2) |
|
Hernia, n |
5 |
15 |
5 |
25 (0.3) |
|
Total, n(%) |
71 (0.9) |
74 (1) |
40 (0.5) |
185 (2.4) |
Duration of operative procedure
The average duration of the operative procedure in all three groups (excluding open cholecystectomy after conversion) was 22 minutes (range 7 to 84). The time of the procedure for the 1st surgical group averaged 30 minutes (range 26 to 84), as compared with 20 minutes (range 21 to 61) for the 2nd groups and 14 minutes (range 7 to 35) for the 3rd group.
The weighted mean duration of 14 minutes for the 3rd group was significantly lower than the mean duration of 30 minutes for the 1st group of patients (p<0.05) (Table 3).
Length of hospital stay
The mean hospital stay for the entire group was three days (range 12 hours to 15 days). The mean hospital stay duration for patients in the Group 1 was 3.9 days, and for patients in the Group 2 - 3.1 days; and was 2.1 days for the patients from Group 3 (p<0.05).
|
Table 3. Outcomes of laparoscopic cholecystectomy |
||||
|
Variables |
Group 1 |
Group 2 |
Group 3 |
p |
|
Conversions, n(%) |
8 (0.5) |
9 (0.4) |
5 (0.3) |
<0.05 |
|
Complications, n(%) |
71 (0.9) |
74 (1) |
40 (0.5) |
<0.05 |
|
Hospital stay, days |
3.9 |
3.1 |
2.1 |
<0.05 |
|
Operation time, min |
29 |
20 |
14 |
<0.05 |
Discussion
Our study demonstrated reduction over time the rate of complications, conversion to cholecystectomy, shortening of hospital stay and operation time of LC.
LC has gained significantly bigger popularity comparing to the traditional surgery. At the same time, any new medical procedure requires serious critical assessment of possible related complications. The lowest mortality rate, however, might be a result of the fact that the patients were a selected population who underwent elective surgery.
The overall rate of bile-duct injury during LC in this group was 0.9%, which is close to those reported in literature (8, 11, 17). It was shown that such type of complications occur at in practice of less experienced surgeons. In our series we did not have cardiac and pulmonary complications reported by other authors (20, 21).
The shortened hospital stay after the LC was accompanied by low readmission rate that also reduced over time and was relatively small - 0.7, 0.5 and 0.4% correspondingly. The short hospital stay was also associated with the early return to normal activities; 6423 (85%) of 7557 patients who underwent LC returned to fulltime employment within 7 days after the surgery.
Reduction over time conversion to conventional cholecystectomy, complication rates, duration of hospital stay and operation time may be related to increase in surgical experience.
Conclusion
As the gathered statistic data shows, the growing surgical experience leads to the decrease of the conversion rate, complications, hospital stay and mean operation time. The present study report represents strong support to the opinion that LC is currently the gold standard for surgical treatment of gallstone disease.
Peer-review: external and internal
Conflict of interest: None to declare
Authorship: R.S., C.D., G.J., A.K., R.B. equally contribute to the study and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

