International scientific -practical conference dedicated to 60 years of the first heart surgery and 15 years of SRIHSOT: Papers and Abstracts
CONFERENCE PAPERS AND ABSTRACTS
International scientific -practical conference dedicated to 60 years of the first heart surgery and 15 years of SRIHSOT: Papers and Abstracts
Article Summary
- DOI: 10.24969/hvt.2019.124
- Page(s): 60-93
- Published: 19/04/2019
- Received: 19/04/2019
- Accepted: 19/04/2019
- Views: 49865
- Downloads: 7944
- Keywords: conference abstracts
Abstracts
A-1
Comparative analysis of the results of VSD closure using ministernotomy and full sternotomy
Sheishenov Zh.O., Joshibayev S.D, Aidarova R.A., Rozbayev Z.N., Alibekov A.A.
“Research-Clinical Center for Cardiac Surgery and Transplantology”, Taraz, Republic of Kazakhstan
Objective: It is known that the main method of treatment of congenital heart defects (CHD) in children is surgical correction. Despite the progress in cardiac surgery, the risk of using open-heart surgery remains high. Therefore, in recent years, much attention has been paid to the introduction of less traumatic methods of surgical CHD treatment. The advantages of mini-accesses are the reduction of surgical trauma, less issues with wound, faster patient recovery and an obvious cosmetic effect.
The aim of the work is to show the results of surgical correction of VSD in children using the access of ministernotomy and full sternotomy.
Methods: the patients were divided into 2 groups: group 1- main group (n-15), operated using the ministernotomy; group 2- control (n-17), operated using full longitudinal sternotomy. The groups were matched by gender, age and diagnosis (18 girls, 14 boys, average age was equal to 3 years).
The indications for the defect plasty using partial sternotomy (in the form of an inverted club) were all types of isolated VSD, except for inlet localization, when right anterior minithoracotomy was used.
We analyzed the results based on main research criteria: the duration of the operation, duration of bypass, discharge volume through the drainage system, the size of the postoperative scar, the subjective status of the patient and the cosmetic effect of the postoperative wound upon discharge and after 3 months.
Results: The study found that there were no significant difference between two above groups in the average operation and bypass time as well as in duration of patient`s stay in the ICU. Moreover, there was no significant difference in the length of the postoperative hospital stay (10 ± 2 days). Healing of wounds in both groups was fast with primary intention.
The main advantage of partial sternotomy were the enhanced recovery of children activity in the early postoperative period and a positive subjective assessment of the size of the wound by parents of patients, especially in the late period, i.e. in 3 months.
Conclusions: we pursued a definite goal of using ministernotomy for closure of VSD to obtain a good cosmetic effect and rapid rehabilitation in the early postoperative period. The results allow us to state that the ministernotomy for the correction of congenital septal defects can be considered as a quite safe and effective surgical access.
A-2
Echocardiographic criteria for the selection of patients for the closure of VSD using right-sided anterior minithoracotomy
Sheishenov Z.O., Joshibayev SD, Mukhamedov I.I, Aidarova R.A, Ustemirov E.B, Ukolova Y.N.,
“Research-Clinical Center for Cardiac Surgery and Transplantology”, Taraz, Republic of Kazakhstan
Objective: In order to close the ventricular septal defect (VSD) under bypass using right-sided anterior minithoracotomy (RAMT), an exact defect characteristic of transthoracic echocardiography (EchoCG) is necessary. Echocardiography visualization during childhood is usually not difficult.
Aim of the study: to determine the criteria for the selection of patients for VSD closure using RAMT based on the EchoCG data assessment
Methods: diagnosis of inlet or outlet VSD, the relationship of the edge of the defect to aortic annulus, the degree of manifestation of the ventriculo-infundibular fold tissue based on the results of two-dimensional EchoCG with pulsed and color Doppler imaging with 5x-1 MHz transducer using Philips IE-33 device. For transthoracic EchoCG, standard positions were used to visualize the interventricular septum, but the basic morphological picture was obtained from two positions. These are parasternal view of the long- and short-axis and four- and five-chamber apical view. When examining patients with VSD, localization, shape and size of the defect, degree of dilatation of the right heart chambers, and degree of pulmonary hypertension were taken into account.
|
|
|
|
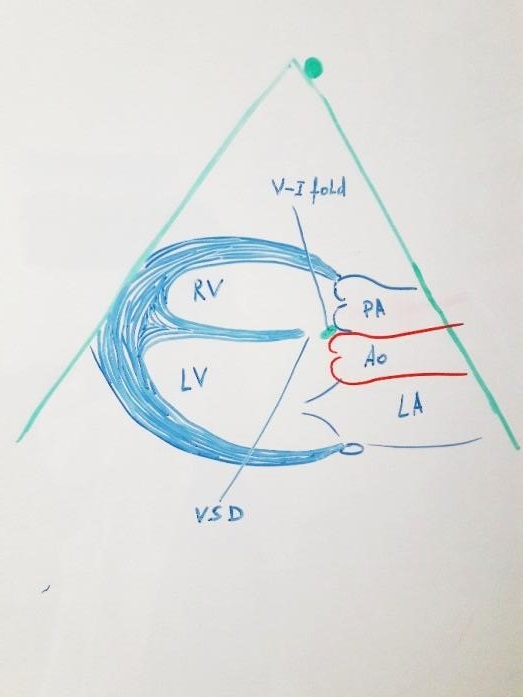
Figure 1. Parasternal long-axis view |
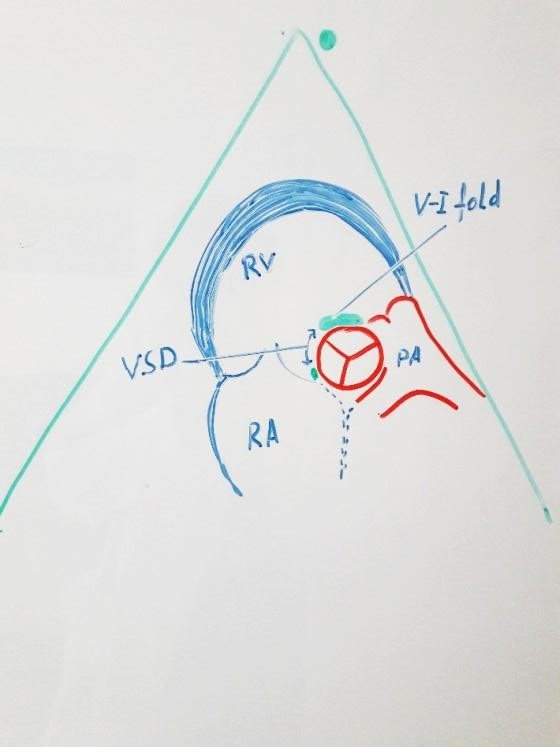
Figure 2. Parasternal short-axis view - aorta |
Results: in Figure 1, the parasternal view is the long axis of the heart is shown, where the tissue of the ventriculo-infundibular fold under the aortic annulus is visible.
The basic information characterizing the inlet VSD is derived from the parasternal view along the short axis of the aorta. This can be seen in Figure 2. If we represent the aortic annulus as a clock face, then we have a shunt blood flow through VSD in the region from 9 to 11 hours, where the defect is completely surrounded by crista supraventricularis.
The outlet VSD is characterized by the visualization of a shunt blood flow between 11 and 13 hours and the absence of the tissue of the ventriculo-infundibular fold, which gives a picture of merging with the aortic annulus or as a narrow slit. While, in case of large VSD, the discontinuity on the interventricular septum extends under the septal leaflet of tricuspid valve up to 12 hours of the aortic annulus.
Conclusion: Transthoracic EchoCG allows assessing the localization, shape and size of the defect, thereby selecting groups of patients for the safe and effective closure of VSD under bypass conditions using RAMT.
AUTHOR'S CORNER