A case of undifferentiated pleomorphic cardiac sarcoma
CASE REPORT
A case of undifferentiated pleomorphic cardiac sarcoma
Article Summary
- DOI: 10.24969/hvt.2021.263
- Page(s): 144-149
- CARDIOVASCULAR DISEASES
- Published: 11/08/2021
- Received: 02/07/2021
- Revised: 10/08/2021
- Accepted: 10/08/2021
- Views: 7727
- Downloads: 6032
-
Citations
- Keywords: cardiac sarcoma, left atrium, left ventricle, right ventricle, metastases, echocardiography, cardiac magnetic resonance, biopsy, autopsy, tamponade
PDF PRINT VERSION CommentsAddress for CorrespondenceAddress for Correspondence: Sergey Yakovlev, Moscow City hospital named after I.V. Davidovsky, Moscow, Russian Federation,
Email: dr.s.yakovlev@gmail.com Mobile: +79161884244
Sergey Yakovlev1, Anna Kalinskaya2
1Moscow City hospital named after I.V. Davidovsky, Moscow, Russian Federation
2Moscow State University of Medicine and Dentistry, Moscow, Russian Federation
Abstract
Primary cardiac sarcoma is known to have a poor prognosis due to late presentation, multiple metastases, and complications, challenging treatment options. We present a case of a 78-year-old female patient who was admitted to our hospital with progressive dyspnea and chest pain. Echocardiography revealed multiple masses of different shape and size in the left atrium, the left and right ventricles. Cardiac magnetic resonance confirmed multiple cardiac masses with signs of invasion in the myocardium and heterogeneous late gadolinium enhancement in all these masses. A biopsy of the abdominal mass revealed an undifferentiated pleomorphic sarcoma.
We planned chemotherapy and supportive measures. Before the initiation of the chemotherapy, the clinical situation worsened dramatically. Despite the pericardiocentesis, the patient died due to cardiac tamponade. An autopsy revealed a massive tumor in the interatrial septum and multiple metastases in both ventricles, lungs, and abdomen.
Key words: cardiac sarcoma, left atrium, left ventricle, right ventricle, metastases, echocardiography, cardiac magnetic resonance, biopsy, autopsy, tamponade
Introduction
Primary cardiac tumors are uncommon (1-3). In case of primary cardiac tumor we should pay special attention to the evaluation of the malignancy (it can be found in 25% of cases). The most common malignant tumor is sarcoma. Primary cardiac sarcoma is known to have poor prognosis due to late presentation, multiple metastases and complications, challenging treatment options (4). The most common cause of death in these patients is heart failure (5).
We present a case of undifferentiated pleomorphic cardiac sarcoma that was complicated by cardiac tamponade. The patient died due to cardiac tamponade.
Case report
A 78-year-old female patient was admitted to our hospital with progressive dyspnea and chest pain, which occurred during minimal physical activity (chronic heart failure NYHA functional class III). She had been diagnosed with hypertension stage 2, diabetes mellitus type 2 several years ago. One year ago, she noticed the dyspnea and chest pain during physical activity. Two months ago, she had an episode of palpitation. The electrocardiography (ECG) revealed atrial fibrillation. Her sinus rhythm was restored with amiodarone. The echocardiography revealed an echogenic mass in left atrium. The myxoma was suspected. Coronary angiography was performed to exclude coronary artery disease. It revealed absolutely normal coronary arteries.
Upon admission, vital signs were unremarkable. The complete blood count revealed hypochromic anemia (hemoglobin, 94 g/L; red blood cell count 3.55 X 10ˆ12 /L).
A round-shaped mass of 1.5 to 2 cm in diameter was palpated at the anterior abdominal wall (mesogastrium). An ECG upon admission to our clinic was normal. Two-dimension echocardiography revealed multiple masses of different shape and size in the left atrium, the left and right ventricles.
The left ventricle ejection fraction was 60–65%; a restrictive type of diastolic dysfunction was observed (Video 1, 2, Fig. 1. Watch videos at www.hvt-journal.com). Cardiac magnetic resonance (CMR) confirmed multiple cardiac masses with signs of invasion in the myocardium and heterogeneous late gadolinium enhancement (LGE) in all these masses (Video 3, 4, Fig. 2 Watch videos at www.hvt-journal.com).
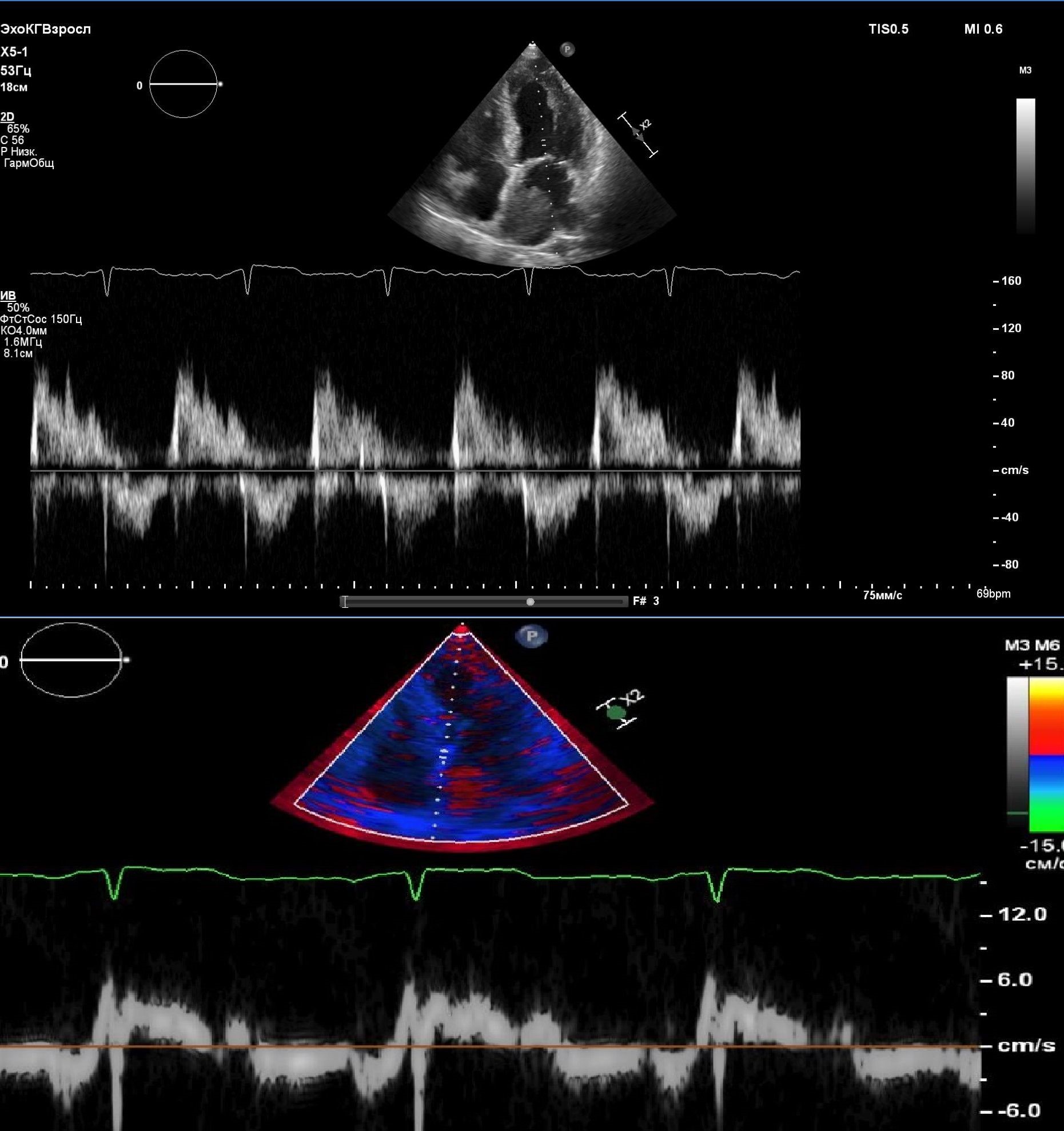
Figure 1. Upper part of the figure- transmitral flow, pulsed wave Doppler. Lower part of the figure- tissue Doppler image of restrictive pattern of transmitral and mitral annular flow.
Video 1. Echocardiography. Apical four-chamber view. Multiple masses in left atrium, left ventricle and right ventricle.
Video 2. Echocardiography. Parasternal long-axis view. Multiple masses in left atrium and left ventricle.
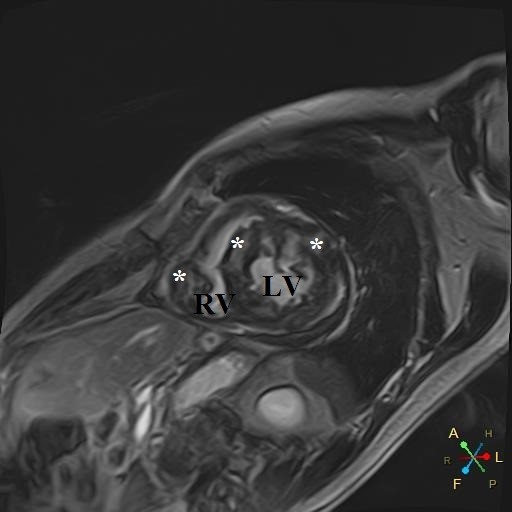
Figure 2. Cardiac magnetic resonance imaging - short axis view of intramyocardial masses with late gadolinium enhancement (*). LV – left ventricle, RV – right ventricle
Video 3. Cardiac magnetic resonance imaging. Four-chamber view. Multiple masses in left atrium, left ventricle and right ventricle
Video 4. Cardiac magnetic resonance imaging. Short-axis view. Multiple masses in left ventricle and right ventricle
A biopsy of the abdominal wall mass was performed. It revealed a low-differentiated malignant tumor. Immunohistochemistry assay confirmed an undifferentiated pleomorphic sarcoma. Figure 3 showed the microscopic appearance of the heart tumor, composed of spindle cells admixed with polygonal or rounded cells, scattered bizarre cells, arranged in a storiform pattern. There were marked cellularity and nuclear pleomorphism with abundant atypical mitoses. Figure 4 showed marked proliferation activity of tumor cells, labeled with Ki67.
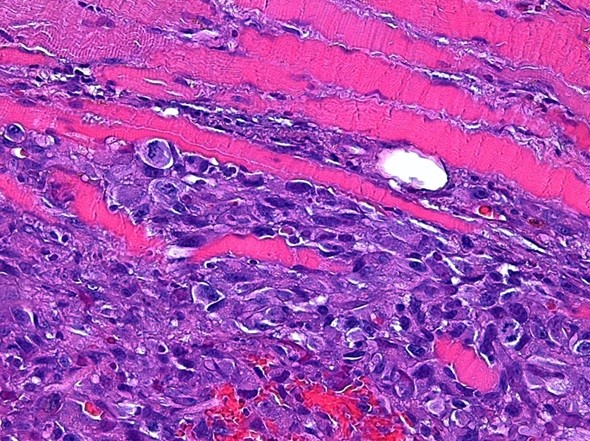
Figure 3. Hematoxylin and eosin stain, magnification 400 – image of heart tumor (See explanation in text).
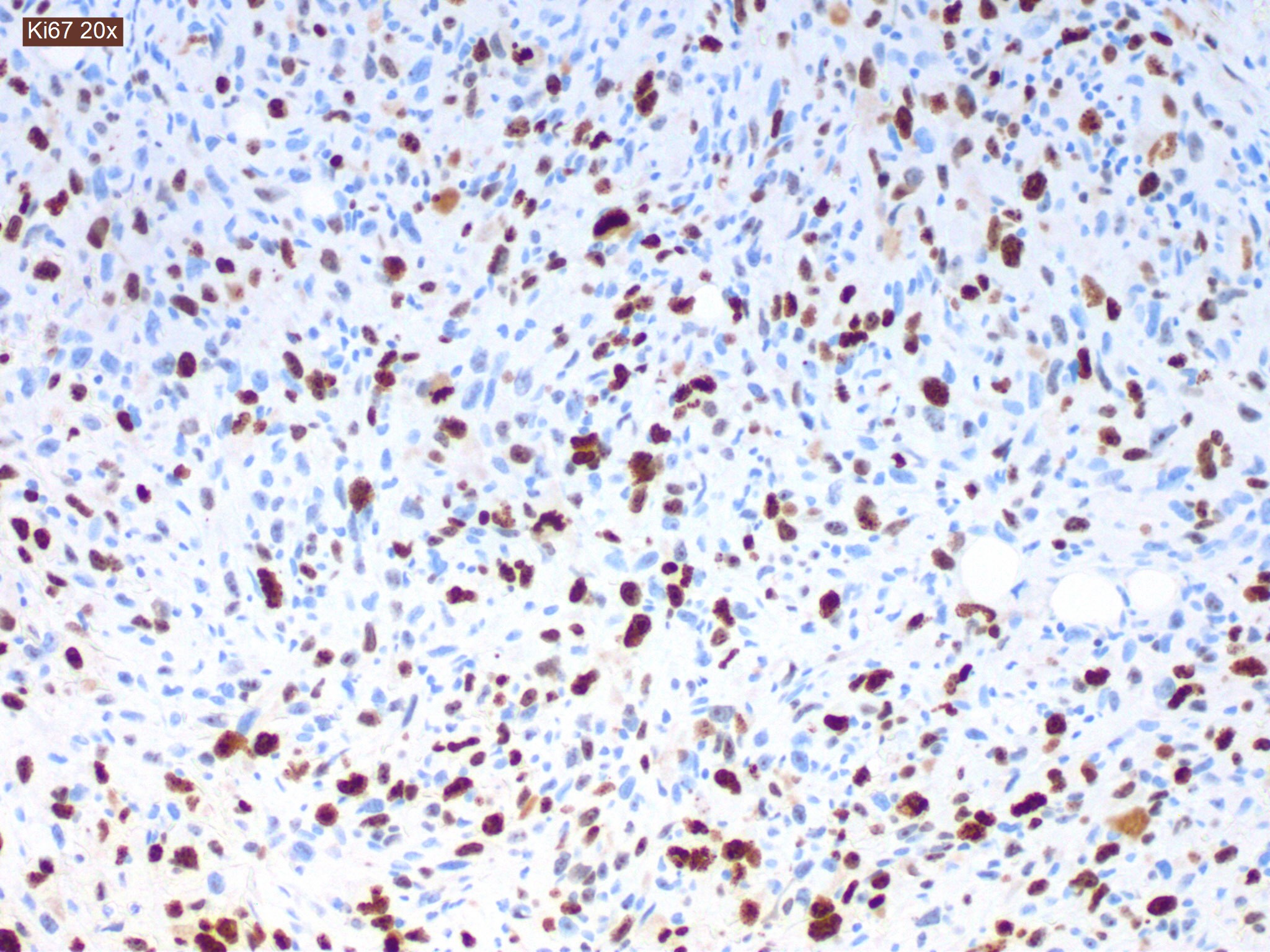
Figure 4. Immunohistochemistry assay, magnification 200 - image of heart tumor (See explanation in text).
Because of the extent of the lesion site (left atrium and both ventricles), the only options for treatment were chemotherapy and supportive measures. Before the initiation of the chemotherapy, the clinical situation worsened dramatically. After the initial episode of severe dyspnea, the patient lost consciousness. The emergency echocardiography showed signs of cardiac tamponade. Despite the pericardiocentesis, the patient died.
An autopsy revealed a massive tumor in the interatrial septum and multiple metastases in both ventricles, lungs, and abdomen (Fig. 5).
Discussion
Primary malignant heart tumors are rare conditions (1-3). Undifferentiated pleomorphic sarcoma (UPS) occurs in 12% cases of primary cardiac sarcoma (6). It is known to be a high-grade malignancy that proliferates rapidly. The median survival time is about 6-12 months (7). The mean age of UPS is known to be about 45 years (8). This case is unusual due to the very late occurrence and clinical presentation of the tumor.
UPS can cause different symptoms such as dyspnea, palpitations, or weakness. In some cases, the first presentations of the tumor can be arrhythmia, i.e. atrial fibrillation, or acute decompensation of patient status (i.e. acute heart failure, life-threatening arrhythmias or tamponade) (9). All these signs and symptoms are not specific. Sometimes UPS can be an accidental finding on echocardiography, computed tomography scan or CMR. In our case the patient had complex clinical presentation: dyspnea, chest pain and atrial fibrillation. Dyspnea and atrial fibrillation in our patient can be caused by diastolic dysfunction of left ventricle due to sarcoma invasion or mitral valve, and pulmonary veins obstruction.
The best treatment strategy is a combination of complete surgical excision, chemotherapy and radiotherapy (10). But UPS is a locally invasive tumor. This makes complete surgical excision often impossible. Even after the complete tumor removal, the relapse rate is very high (11). Heart or heart-lung transplantation can be an option, but this procedure does not significantly change survival and often has a high risk (12, 13). There are no exact protocols for chemotherapy and radiotherapy in such a case, different combinations can be used (14).
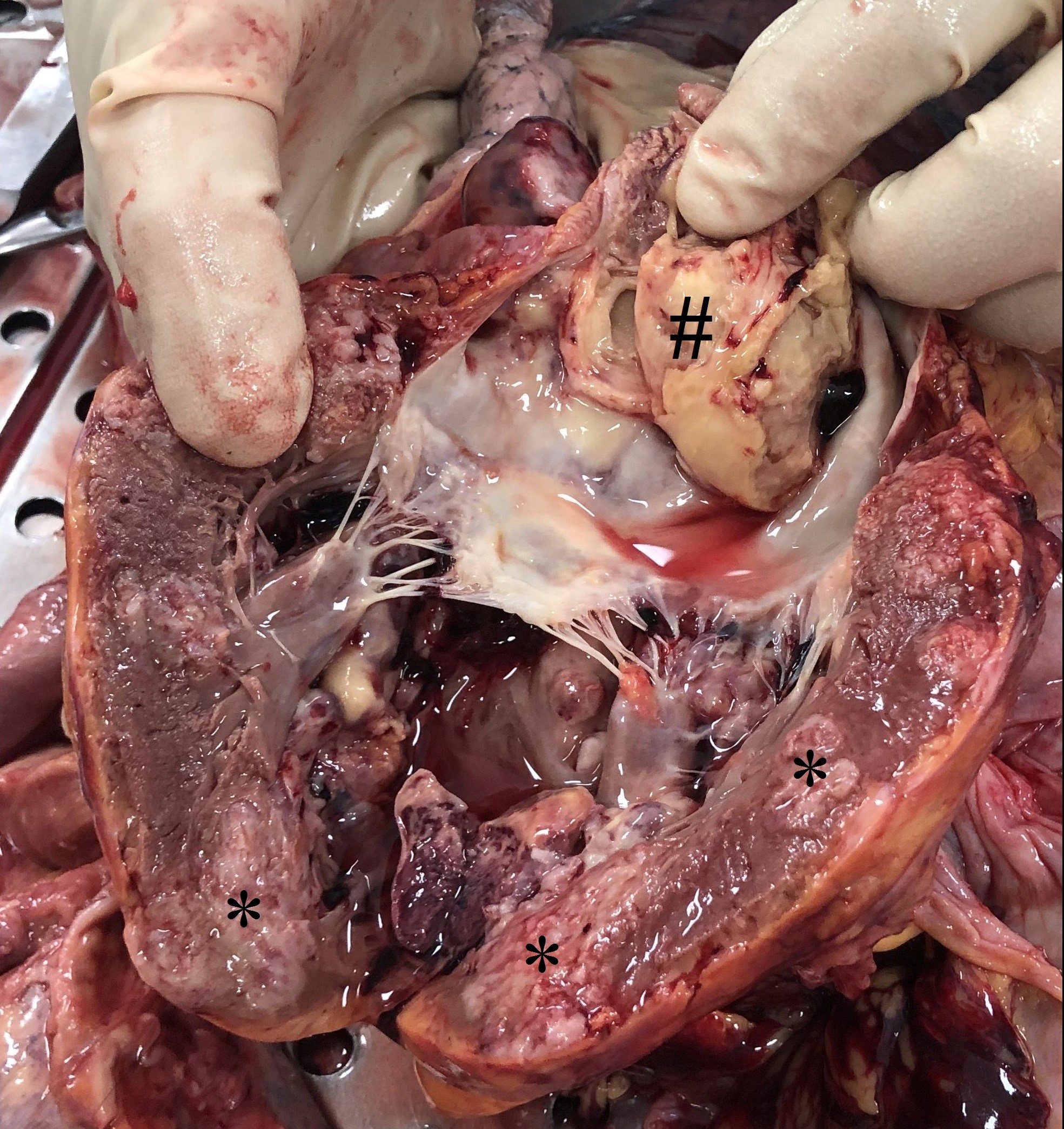
Figure 5. Autopsy. Opened left ventricle and left atrium. # - mass in the left atrium, * - intramyocardial metastases in left ventricular wall
Our patient had a grave prognosis as she had multiple intracardiac and extracardiac metastases that made the surgical excision and heart transplantation unsuitable. Thus, we planned to perform chemotherapy. Unfortunately, the patient developed the acute cardiac tamponade that led to the death despite the pericardiocentesis. The acute cardiac tamponade is an extremely dangerous condition that can be caused by different reasons: cardiac muscle rupture due to myocardial infarction; coronary artery perforation, systemic disease and etc. The cardiac tumors should also be under the consideration.
Conclusion
Undifferentiated pleomorphic sarcoma is an extremely rare disease. Presentation of UPS can be different: from silent cases with accidental findings to acute deterioration (heart failure, arrhythmias, cardiac tamponade). Treatment is challenging and prognosis is often poor. The preferable treatment option is a combination of surgery, chemotherapy and radiotherapy.
Ethics: Informed consent and permission of patient was obtained for all procedures
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: S.Y. and A.K. are equally contributed to case management and preparation of article
Acknowledgments and funding: None to declare
References
1.Reynen K. Frequency of primary tumors of the heart. Am J Cardiol 1996; 77: 107. https://doi.org/10.1016/S0002-9149(97)89149-7 2.Nomoto N, Tani T, Konda T, Kim K, Kitai T, Ota M, et al. Primary and metastatic cardiac tumors: echocardiographic diagnosis, treatment and prognosis in a 15-years single center study. J Cardiothorac Surg 2017; 12: 103. https://doi.org/10.1186/s13019-017-0672-7 3.Cresti A, Chiavarelli M, Glauber M, Tanganelli P, Scalese M, Cesareo F, et al. Incidence rate of primary cardiac tumors: a 14-year population study. J Cardiovasc Med 2016; 17: 37-43. https://doi.org/10.2459/JCM.0000000000000059 4.Brittany LS, Zhao L, Leja M, McHugh JB, Shango MM, Baker LH, et al. Primary cardiac sarcoma: a rare, aggressive malignancy with a high propensity for brain metastases. Sarcoma 2019; 1960593 5.Donsbeck WK, Ranchere D, Coindre JM, Le Gall F, Cordier JF, Loire R. Primary cardiac sarcomas: an immunohistochemical and grading study with long-term follow-up of 24 cases. Histopathology 1999; 34: 295-304. https://doi.org/10.1046/j.1365-2559.1999.00636.x 6.Randhawa JS, Budd GT, Randhawa M, Ahluwalia M, Jia X, Daw H. Primary cardiac sarcoma: 25-year Cleveland Clinic experience. Am J Clin Oncol 2016; 39: 593-9. https://doi.org/10.1097/COC.0000000000000106 7.Vallés-Torres J, Izquierdo-Villarroya MB, Vallejo-Gil JM, Casado-Domínguez JM, Roche Latasa AB, Auquilla-Clavijo P. Cardiac undifferentiated pleomorphic sarcoma mimicking left atrial myxoma. J Cardiothorac Vasc Anesth 2019; 33: 493-6. https://doi.org/10.1053/j.jvca.2018.02.010 8.Oliveira GH, Al-Kindi SG, Hoimes Ch, Park SJ. Characteristics and survival of malignant cardiac tumors. A 40-year analysis of >500 patients. Circulation 2015; 132: 2395-402. https://doi.org/10.1161/CIRCULATIONAHA.115.016418 9.Kim DM, Hong JH, Kim SY, Yoo KD, Seo JY, Rhee KJ, et al. Primary cardiac angiosarcoma presenting with cardiac tamponade. Korean Circ J 2010; 40: 86-9. https://doi.org/10.4070/kcj.2010.40.2.86 10.Kong PK, Theodorou S, Beran E, Singh H, Dimitri W. Primary cardiac undifferentiated sarcoma of the right atrium presenting with cardiac tamponade. Cardiovasc Pathol 2009; 18: 110-3. https://doi.org/10.1016/j.carpath.2007.10.006 11.Truong PT, Jones SO, Martens B, Alexander C, Paquette M, Joe H, et al. Treatment and outcomes in adult patients with primary cardiac sarcoma: the British Columbia Cancer Agency experience. Ann Surg Oncol 2009; 16: 3358. https://doi.org/10.1245/s10434-009-0734-8 12.Li H, Yang S, Chen H, Yang Zh, Hong T, Hou Y, et al. Survival after heart transplantation for non-metastatic primary cardiac sarcoma. J Cardiothorac Surg 2016; 11: 145. https://doi.org/10.1186/s13019-016-0540-x 13.Mazuecos JMJ, Manso RF, Cubero JS, Ramos JT, Domínguez JFO, Rivera LAP. Is heart transplantation for primary cardiac sarcoma a useful therapeutic option? Rev Esp Cardiol 2003; 56: 408-11. 14. Patrikidou A, Domont J, Cioffi A, Le Cesne A. Treating soft tissue sarcomas with adjuvant chemotherapy. Curr Treat Options Oncol 2011; 12: 21-31. https://doi.org/10.1007/s11864-011-0145-5

Delfshaven, Rotterdam. The Netherlands – March 2021. Jonathan Lipton, Melbourne, Hobart, Tasmania, Australia
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.Archive of Issues
AUTHOR'S CORNER
 Authors having problems with submissions please notify editor: editor@hvt-journal.com
Authors having problems with submissions please notify editor: editor@hvt-journal.com
