Blunt traumatic aortic injury: CT angiography images and short review of current literature
REVIEW
Blunt traumatic aortic injury: CT angiography images and short review of current literature
Article Summary
- DOI: 10.24969/hvt.2021.287
- Page(s): 184-189
- Published: 17/11/2021
- Received: 19/10/2021
- Revised: 13/11/2021
- Accepted: 14/11/2021
- Views: 8330
- Downloads: 5370
- Keywords: lunt traumatic aortic injury, CT angiography, pseudoaneurysm, aortic rupture, aortic isthmus injury, TEVAR
Address for correspondence: Ferhat Can Piskin, Department of Radiology, Cukurova University Faculty of Medicine, Balcali Hospital, Adana, Turkey
E-mail ferhatcpiskin@gmail.com Mobile: +90 555 736 82v83
Ferhat Can Piskin1, Duygu Ozgul1, Yasin Guzel2, Erol Huseyin Aksungur1
1Department of Radiology and 2Department of Cardiovascular Surgery, Cukurova University Faculty of Medicine, Balcali Hospital, Adana, Turkey
Abstract
Blunt traumatic aortic injury in high-energy motor vehicle accidents is a rare but life-threatening condition. Proper treatment after prompt and accurate diagnosis is critical to reduce the death rate. The purpose of this article was to highlight the points to be considered in blunt traumatic aortic injury due to high-energy motor vehicle accident.
Key words: Blunt traumatic aortic injury, CT angiography, pseudoaneurysm, aortic rupture, aortic isthmus injury, TEVAR
Introduction
Blunt traumatic aortic injury (BTAI), seen in 3-17% of high-energy motor vehicle accidents, is a rare but life-threatening condition (1, 2). BTAI is the second most common cause of traumatic death after brain injury with an incidence of 10-20%. Most of the deaths occur before the patient can reach the hospital (3). In addition, BTAI can easily be overlooked without diagnosis, since most of the patients who reach the hospital have non-specific physical examination findings and other accompanying injuries cause symptoms that are more prominent (4).
The purpose of this article was to highlight the points to be considered in blunt traumatic aortic injury due to high-energy motor vehicle accident.
Case one
A 24-year-old male patient who was brought to the emergency department after a motorcycle accident was evaluated with multiple trauma protocol that covers upper and lower abdomen computed tomography (CT) examinations performed after approximately 70cc intravenous contrast material injection at a rate of 4ml/sec after non-contrast brain, spinal and thorax CT). In the first physical examination, the patient was unconscious, blood pressure was 110/85 mmHg, heart rate was 88 beats/min and respiratory rate was 25/min. There were abrasion and ecchymotic areas on the scalp and anterior chest wall.
On CT examination, areas of hemorrhagic contusion in the bifrontal deep white matter in the brain, foci of intraventricular bleeding were detected. In addition, non-contrast thorax CT showed widening of the mediastinal borders and high-density fluid compatible with hematoma around the aortic arch (Fig. 1). Contrast-enhanced arterial phase CT angiography (CTA) was performed with the suspicion of thoracic aortic injury due to the detected findings. On CTA; a full-thickness vessel wall rupture starting from the left subclavian artery orifice at the level of the arcus aorta isthmus and continuing for 5 cm was observed (Fig. 2). Due to hemodynamic instability, open surgery was preferred over thoracic endovascular aneurysm repair (TEVAR). The patient was taken to open surgery by the cardiovascular surgery team, intubated and the tear in the aorta was repaired with a 26 mm Dacron graft.
The patient was followed up in the intensive care unit after the operation. On the 16th day of the trauma, the patient general condition deteriorated and blood pressure continued to decrease under maximum inotropic support. Cardiac arrest developed and death occurred despite adequate life support therapy.

Figure 1. On non-contrast thorax computed tomography (axial images), a hematoma is observed in the mediastinum and around the aorta
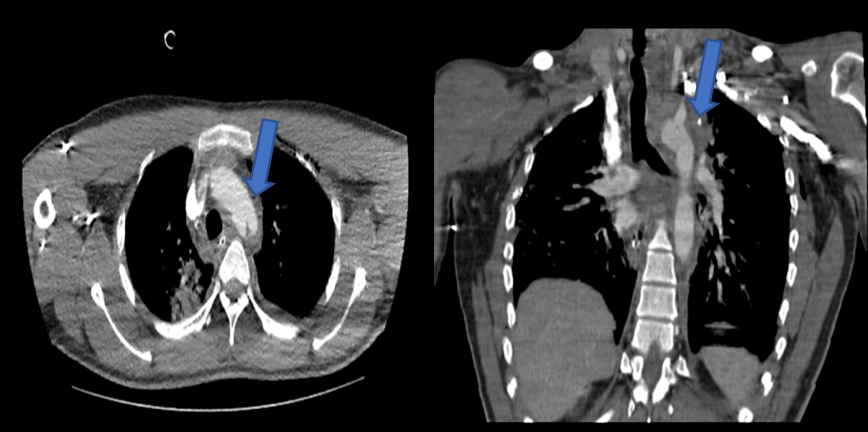
A) B)
Figure 2. On contrast-enhanced computed tomography of the thorax (axial (a) and coronal (b) images), a complete rupture of the aortic arch at the level of the isthmus is observed (blue arrow).
Case two
A 50-year-old male patient who was brought to the emergency department after a traffic accident without any additional disease history was examined upon the detection of multiple, segmented, open fractures in the lower extremity and accompanying chest pain in the initial evaluation. The patient was conscious, blood pressure was 135/85 mmHg, pulse was 77 beats/min, and respiratory rate was 17/min.
Chest examination on non-contrast CT revealed hemopneumothorax on the left and accumulation of fluid consistent with mediastinal high-density hematoma. In addition, a 2 cm wedge-shaped segmental infarction area, which was thought to have developed on the ground of arterial embolism, was detected in the lower pole of the right kidney in the abdominal examination with intravenous contrast.
CT angiography was performed with suspicion of lower extremity arterial injury and aortic injury. CT angiography showed pseudoaneurysms that started 6 mm distal from the left subclavian artery orifice and reached 2 cm in diameter (Fig. 3). In the left tibioperoneal trunk, a filling defect compatible with a partially canalized thrombus was noted. The patient, whose vital signs remained stable during the follow-up but had a decrease in hematocrit values, was treated by the cardiovascular surgery team with TEVAR method. Pseudoaneurysms were repaired with a stent-graft extending from the arcus aorta to the descending aorta. No filling was found in pseudoaneurysms on control examinations. Mediastinal hematoma and left hemothorax findings improved. There was no decrease in hematocrit values during follow-up. The follow-up of the patient, who underwent multiple operations for lower extremity fractures, continues.
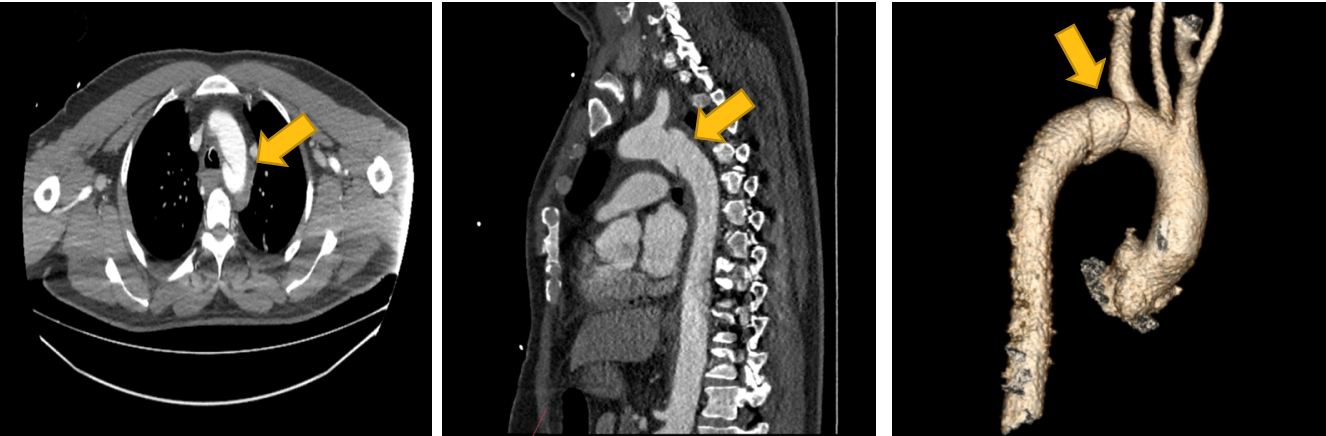
- B) C)
Figure 3. On contrast-enhanced, computed tomography angiography of the thorax (axial (a), coronal (b) and volume rendering (c) images), a saccular structure compatible with a pseudoaneurysm is seen in the isthmus part of the arcus of aorta (yellow arrow)
Discussion
Undiagnosed and untreated BTAI has a high mortality rate of 90%, therefore; accurate diagnosis and appropriate treatment for BTAI is so important (4). According to the guideline published by the American Society of Vascular Surgery (SVS) in 2011, based on BTAI radiological imaging findings; aortic injury is classified from minimal injury to severe aortic injury and is handled in 4 four grades (5). Minimal aortic injuries refer to sub-centimetric intima-media injuries that do not show external contour irregularity in the vascular wall (6-8). This group includes small (<1 cm) intimal tears (grade I) and intramural hematomas (grade II). Significant aortic injuries are defined as pseudoaneurysms (grade III) and aortic rupture (grade IV) (9).
The aortic isthmus is the most frequently injured part in BTAI, followed by the aortic root and the abdominal aorta at aortic hiatus level. The frequent occurrence of injury at these levels is associated with greater immobility/fixation of these areas compared to other parts of the aorta (10-12). Although the mechanisms of injury to the aorta by blunt trauma are still controversial, rapid deceleration (stretching), osseous compression, shear and hydrostatic forces (water hammer effect) are considered as possible mechanisms. Rapid deceleration (stretching) is an example of the mechanism of injury of the aortic arch, which is subjected to the opposite vertical tension force of the branches of the cranial arch and the caudal heart and intercostal arteries. The osseous compression mechanism explains the aortic injury that occurs as a result of compression between the rigid structures of the sternocostal joint and the vertebral column. The shearing effect is associated with aortic injury because of tensile and torsion forces to which the fixed/immobile points of the aorta, such as the aortic isthmus, are exposed. In the mechanism called hydrostatic forces (water hammer effect), increased intraluminal pressure after blunt trauma is blamed. Although the exact contribution of different forces is not known, convergence/combination of more than one force is considered as a possible theory in the formation mechanism of BTAI (13, 14).
Multiphase CT angiography examination including non-enhanced, arterial and venous phases is sufficient for diagnosis. Non-contrast images are recommended for identifying vessel wall hematoma, arterial phase images for optimal evaluation of the lumen, and venous phase images for revealing possible dissection that shows slow filling and cannot be differentiated from thrombus in arterial phase (15). ECG-triggered examinations are particularly preferred to distinguish injuries at the ascending aorta level from pulsation artifacts. However, ECG-triggered CTA examination is not necessary for this group of patients, because BTAI often develop in the descending thoracic aorta and abdominal aorta (16).
In patient management after diagnosis, open surgery or TEVAR can be preferred. Minimal aortic injuries classified as grade I according to SVS can be followed up without treatment by serial imaging methods by providing blood pressure and pulse control (pulse <70-80 beats / min, systolic pressure <110-120 mmHg). However, if there are accompanying traumas such as cerebral and spinal injuries that prevent the control of blood pressure and pulse during follow-up, treatment may become mandatory. Low-dose heparin treatment is preferred due to the risk of distal embolism that may develop in the background of turbulent flow. There is no consensus on the treatment of aortic pseudoaneurysms that develop as a result of blunt trauma. There are opinions arguing that pseudoaneurysms less than 1 cm can also be followed by serial imaging (17-19). In opposing opinions, the treatment of pseudoaneurysms with TEVAR is advocated regardless of their size (19). Treatment is mandatory in significant aortic injuries for grade III and IV according to SVS (5).
Although open surgery is the traditional and most commonly preferred method, the use of TEVAR, which is less invasive, has increased in recent years. During traditional open repair, procedures such as open thoracotomy, one-lung ventilation, aortic clamping, heparinization, which expose the patient group to more risk, are applied and patients need multiple blood product transfusions (21-23). In a 20-year meta-analysis, mortality and paraplegia rates after open surgical repair were reported as 32% and 9.9%, respectively (24). Prolongation of aortic clamping time in open surgery may result in paraplegia by affecting spinal cord nutrition on the basis of arterial hypotension and increased cerebrospinal fluid (CSF) pressure (25). However, some patients are not anatomically suitable for TEVAR, which limits the applicability of this method. Due to the lack of sufficient landing zone between the ostium of the left subclavian artery and the lesion that needs to be treated, the ostium of the subclavian artery can be closed by a stent-graft. It is known, that left subclavian artery closure can be tolerated in young patients, but can also result in cerebellar infarction.
There is evidence from meta-analyses that CT examination in the multiple trauma protocol in high-energy trauma patients increases survival compared to the selective imaging method for trauma (26, 27). CT evaluation in the multiple trauma protocol generally includes non-contrast brain and cervical vertebra CT, contrast-enhanced thorax and abdomen/pelvis CT, non-contrast multiplanar thoracic and lumbar vertebra CT examinations, although protocols may show different shapes according to medical centers. In our center, thorax imaging is frequently performed without contrast, in the protocol that is widely accepted in adult multiple trauma patients. This situation brings the importance of indirect findings to a critical point in BTAI.
The aortic isthmus was affected in two presented patients. Both patients were classified with presence of as significant aortic injury. In the first case, there was a grade IV injury, namely aortic rupture, according to SVS, while there was a grade III injury with pseudoaneurysms in the second case. In the first case, the injury resulted in mortality as a result of multiple factors such as concomitant cerebral trauma making blood pressure and pulse control difficult, grade IV blunt traumatic aortic injury and the need for open surgical intervention. In the second case, after the detection of grade III blunt traumatic aortic injury, complete repair was achieved with endovascular treatment applied without delay. Distal embolism due to turbulent flow formed on the basis of pseudoaneurysms resulted in renal segmental infarction and partial canalized thrombus in the infrapopliteal arterial structures of the left lower extremity in the second case. Upon detection of indirect signs of aortic damage (periaortic/mediastinal hematoma, aortic contour irregularity, change in aortic calibration, hemothorax) in both cases, aortic injury was detected without delay by CTA examination, management strategies were defined and patients were referred for treatment.
Conclusion
Blunt traumatic aortic injury in high-energy motor vehicle accidents is a rare but life-threatening condition. Early diagnosis, clinician-radiologist collaboration with (multidisciplinary approach) and correct treatment significantly reduce mortality. The role of the radiologist is critical in making the diagnosis without wasting time with appropriate imaging tests in order not to miss the indirect findings of blunt traumatic aortic injury. The current classification of blunt traumatic aortic injuries, regulated by the guideline published by SVS, greatly influences patient management and treatment planning. In terms of treatment methods, TEVAR has been considered as a frequently preferred method in recent years.
Ethics: Informed consent was obtained from the patients’s family before all procedures
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: F.C.P., D.O., Y.G. and E.H.A. are equally contributed to patients` management and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Blue-footed booby (Sula nebouxii), Galapagos Ireland, 2021. This smart bird is distinguished by blue foot due to a fish diet rich of carotenoids, it is an excellent divers and is called booby (Spanish bobo -foolish) because of the awkward walking (www.nationalgeographic.com, www.latin2travel.com). Anna Zelek, Washington, USA.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

