Orthostatic hypotension in elderly: Do you measure orthostatic and clinostatic blood pressure?
EDITORIALS
Orthostatic hypotension in elderly: Do you measure orthostatic and clinostatic blood pressure?
Article Summary
- DOI: 10.24969/hvt.2022.349
- Page(s): 164-167
- CARDIOVASCULAR DISEASES
- Published: 08/11/2022
- Received: 01/11/2022
- Revised: 06/11/2022
- Accepted: 06/11/2022
- Views: 8113
- Downloads: 4166
- Keywords: Orthostatic hypotension, autonomic dysfunction, syncope, falls, hypertension, elderly, frailty
Address for Correspondence: Stefano Cacciatore, Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS
L.go A. Gemelli 8, 00168, Rome, Italy
Email: stefanocacciatore@live.it
Stefano Cacciatore1, Luigi Spadafora2, Francesco Landi1
1Department of Geriatrics and Orthopedics, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, L.go Agostino Gemelli 8, Rome, Italy
2Department of Clinical, Internal Medicine, Anesthesiology and Cardiovascular Sciences, Sapienza University of Rome, Italy
In this article we highlighted the blood pressure management in elderly patients with orthostatic hypotension.
Key words: Orthostatic hypotension, autonomic dysfunction, syncope, falls, hypertension, elderly, frailty
The latest issue of Heart, Vessels and Transplantation featured an interesting article on ambulatory blood pressure monitoring in children and adolescents (1). When reading that, the Geriatrician would immediately put their effort into a compelling closing for their patients. In this spirit, the present editorial focuses on the importance of screening for orthostatic hypotension (OH), especially in older adults. Do you measure orthostatic and clinostatic blood pressure (BP)?
Definition and epidemiology
OH is defined as a reduction in systolic BP of at least 20 mmHg or in diastolic BP of at least 10 mmHg within three minutes of standing. It is a common condition in older adults, with prevalence ranging from 5% in individuals <50 years old to 30% in patients >70 of age. It is responsible for adverse events (i.e., falls, hospitalization, institutionalization), morbidity and mortality (2).
Pathophysiology of orthostatic hypotension
Baroceptor reflex is a homeostatic mechanism that allows to maintain BP at almost constant levels in response to “orthostatic stress”. When moving from laying to standing, 500-800 mL of blood shift to the venous compartment of lower limbs causing a reduction in ventricular preload, stroke volume and, eventually, a decrease in BP. Baroceptors located in the carotid artery and in the aortic arch activate autonomic reflexes and produce increase in heart rate (HR) and in the vascular tone of venous compartment. (2)
OH has a multifactorial etiology. In elderly, arterial stiffness is one possible factor compromising mechanisms of response to BP variability (3). Beside paraphysiological changes, the causes of OH can be broadly divided into primary and secondary, acute and chronic, neurological and non-neurological. Primary OH is caused by several conditions in which patients have a generalized impairment of autonomic functions, among these it is worth to mention: pure autonomic failure, multiple system atrophy, Parkinson’s disease, Lewy body dementia, autoimmune autonomic ganglionopathy. Secondary causes of OH involve diabetes mellitus, cardiovascular diseases, renal failure, venous pooling, postprandial hypotension, intravascular volume depletion, endocrine diseases, sepsis or acute infections (2).
Among secondary causes of OH, a prominent role is played by iatrogenic forms, thus polypharmacology is associated with a significant risk of hospitalization due to fall (4). Over 250 medications, including those prescribed for common conditions, are associated with OH (5, 6). Drugs potentially associated with sympathetic inhibition are anti-depressants, benzodiazepines, anti-psychotics, opioids, and trazodone, while the ones acting on cardiovascular system are nitrates, alpha-blockers, beta-blockers, diuretics, and calcium antagonists. A meta-analysis of clinical trials versus placebo performed by Bhanu et al. (7) suggests that drugs having multiple targets may carry a cumulative risk.
Although the relationship between SARS-CoV-2 infection and OH has not been fully clarified yet, several evidence address autonomic dysfunction as part of long COVID-19. Three possible mechanism of autonomic damage sustained by SARS-CoV-2 infection are hypothesized – i.e., hypovolemia due to deconditioning of the heart and dysregulation of renin-angiotensin-aldosterone system, neurotropism of the virus, and inflammation and development of autoimmunity (8).
Screening and diagnosis
A large study conducted in the United Kingdom showcased lower incidence of OH reported among general practitioners than outlined by previous works. Authors hypothesize this result may be due to an underestimation cause by a lack of time during routine clinical examination or poorly standardized methods of measurement (9).
A proposed screening algorithm is shown in Figure 1. An initial assessment of OH begins by checking medical history for possible risk factors, such as age, medical conditions, medications, history of falls, dizziness or syncope, other autonomic signs and symptoms (i.e., confusion, weakness, visual changes, diaphoresis, pallor), dehydration or heat exposure, prolonged bed rest, or alcohol consumption. American Heart Association (10) endorses the screening between older adults for OH by evaluating postural vital signs. First, the patient should be asked to lay in supine position and BP and HR should be measured after 3-5 minutes. After that, the patient is told to sit, and measurement is done after 1 minute. Eventually, the patient is asked to stand and BP and HR are measured immediately after the patient has stood up, then repeated after 3 minutes. During every postural change, the patient should be put back in bed in case of severe hypotension (≤ 90/60 mmHg) and autonomic signs and symptoms. A drop in systolic BP of at least 20 mmHg or in diastolic BP of at least 10 mmHg within three minutes of standing may suggest OH. An increase in HR of at least 30 bpm after standing may indicate hypovolemia, independently from the presence of OH. A reduction in BP immediately after standing does not imply OH if a normalization occurs within 3 minutes. If there is a strong suspect of OH, but a single measurement tests negative, another postural vital signs assessment can be performed either when the symptoms occur or within 2 hours after the start of a meal (10, 11). Laboratory testing, such as blood count, electrolytes, glucose, renal function, and thyroid function may help rule out secondary causes. Further medical examination may include ambulatory BP monitoring, whereas electrocardiogram (ECG), echocardiography, dynamic ECG Holter can be used to rule out cardiogenic syncope. Head up tilt test can be used to rule out vasovagal syndrome when the diagnosis is unclear (12).
Management
Managing OH in older patients is a significant challenge, as impaired BP control, chronic conditions and medications are often responsible for the “Hyp-Hyp phenomenon”, that is the association of OH and clinostatic hypertension (13).
Patients should be educated on avoiding prolonged immobilization and sudden postural changes, large meals, prolonged standing, exposure to high environmental temperature and humidity. Physical countermaneuvres such as legs crossing, muscle tensing and squatting may help rising central BP during standing and prodromal symptoms. Increased salt and fluid intake should be suggested, as well as elastic stockings to reduce peripheral pooling.
Pharmacological interventions include midodrine (2.5–10 mg 2 or 3 times per day), droxidopa (100–600 mg 3 times per day), pyridostigmine (30-60 mg 2 or 3 times per day), fludrocortisone (0.05–0.3 mg daily), Ephedrine/pseudoephedrine (25/30–50/60 mg 3 times per day), desmopressin (nasal spray, 5–40 μg daily; oral formulation, 100–800 μg daily) (2, 14).
In addition, an emerging hot topic is the use of sodium glucose co-transporter 2 (SGLT-2) inhibitors, firstly tested as antidiabetic agents and now endorsed by current guidelines as first line treatment for heart failure, to tame the risk of OH by reducing autonomic dysfunction; their action on glucose homeostasis and inflammation may enhance a better autonomic response to clinostatic stress (15).
The Systolic Blood Pressure Intervention Trial (SPRINT) demonstrated clear benefits in intensive control of systolic BP (≤120 mmHg) on cardiovascular risk, despite a higher risk of OH (16). Other evidence suggests that an optimal control of systolic BP may reduce OH and risk of falls, due to a possible improvement in hemodynamics and baroreflex sensitivity (10). The truth may lie somewhere in between, as the patients may benefit more from gradual titration, regular monitoring and careful assessment rather than from fear of anti-hypertensive drugs. In post-COVID-19 patients, additional management strategies include physical training to avoid chronicity of symptoms (8).
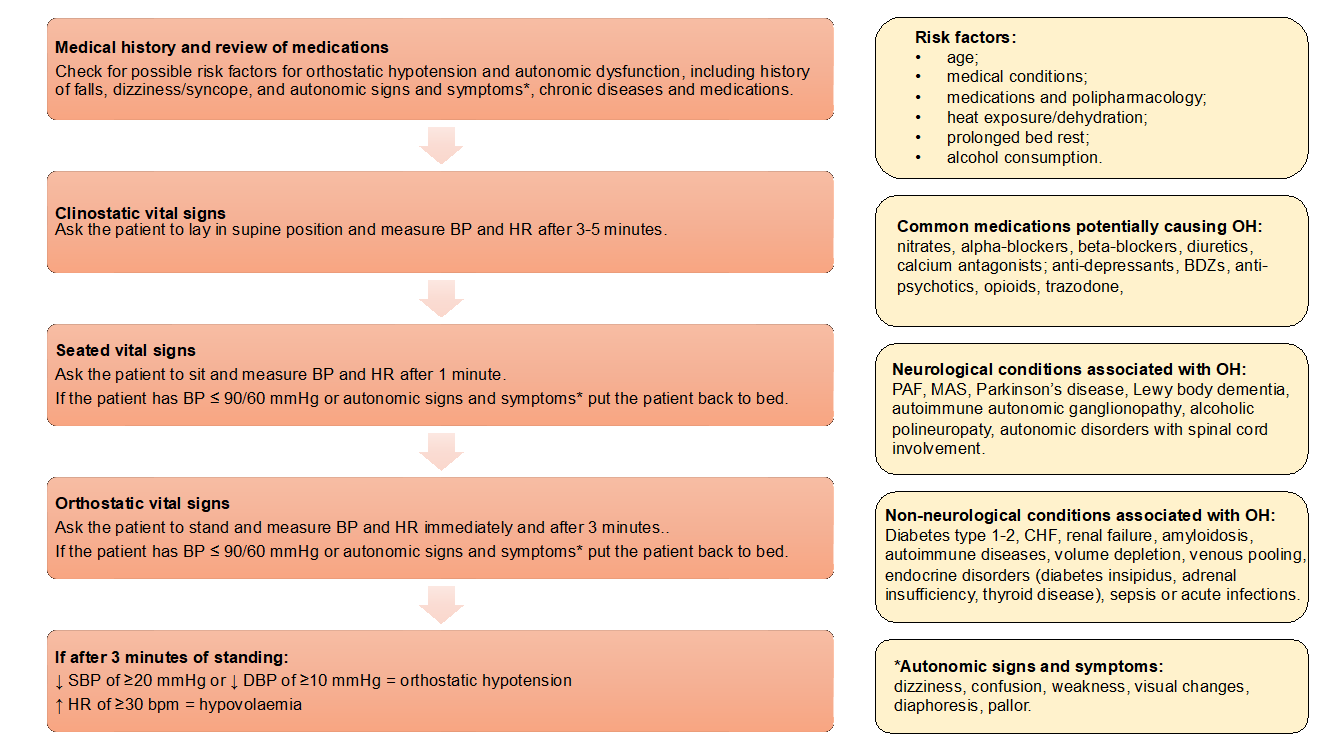
Figure 1. Proposed algorithm for the screening of orthostatic hypotension
BP - blood pressure, DBP - diastolic blood pressure, HR - heart rate, SBP - systolic blood pressure
Figure 2. Practical tools to adopt when clinically approaching a case of orthostatic hypotension
Nutritional supplementation has shown benefits on other long COVID-19 symptoms, such as fatigue (17). Occasional anti-hypertensive drugs at bedtime can be considered for severe clinostatic hypertension (13).
Conclusion
OH is a frequent but often overlooked condition in older adults. Elderly patients present several risk factors for autonomic dysfunction, furthermore drugs administered should be carefully gauged in detail keeping only those strictly essential. In addition, screening and properly training the patient in the management of autonomic dysfunction may have a positive impact on falls, fear of falling and other consequences of OH in terms of quality of life, morbidity and mortality (Fig. 2).
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: All authors have participated in manuscript design and drafting. All authors read and approved the final version.
Acknowledgement and funding: None to declare Authors’ disclosure: The authors have not declared a specific grant for this work from any funding agency in the public, commercial or not-for-profit sectors.
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

