From Editor-in-chief: Our issue, journal`s performance and indexing, new trials, guidelines and consensus documents, long COVID
EDITORIALS
From Editor-in-chief: Our issue, journal`s performance and indexing, new trials, guidelines and consensus documents, long COVID
Article Summary
- DOI: 10.24969/hvt.2023.392
- Published: 29/05/2023
- Received: 28/05/2023
- Accepted: 29/05/2023
- Views: 4832
- Downloads: 4269
- Keywords: editorial
Address for Correspondence: Gulmira Kudaiberdieva, Editor-in-Chief, Heart, Vessels and Transplantation
E-mail: editor@hvt-journal.com

From Editor-in-chief: Our issue, journal`s performance and indexing, new trials, guidelines and consensus documents, long COVID
Dear readers,
In this June 2023 issue of the journal, we brought to your attention articles that contribute to the pool of evidence-based knowledge and also have a value for your practice: research articles on effects of PBMV effects on myocardial performance with discussion of its results, interesting case series sharing the experience on lead removal and replacement of devices in patients with CIEDs and superior vena cava syndrome; the article on stroke dynamics in Bishkek; comprehensive review of evidence on transcatheter interventions in women with valvular heart diseases; interesting case reports that share treatment of challenging cases- simultaneous Bentall procedure and repair of pectus excavatum; surgery for juxta-ductal aorta coarctation and post-coarctation aneurysm and endovascular/ interventional management of a patient with COVID with a history of renal stenosis stenting who developed in-stent thrombosis; articles for your continuous medical education and updates on latest recommendations for clinical practice - quiz article for evaluation of congenital heart diseases, editorials comments on practical use of echocardiography in evaluation of congenital heart diseases developed by British Society of Echocardiography, how to evaluate and treat patients with amyloidosis and anesthesia management of pregnant patients undergoing surgery and two very interesting historical notes on contribution to Vivien Thomas to the treatment of tetralogy of Fallot and his fight against discrimination in science – thus contributing to initiative on inclusion of Vivien Thomas in the name of Blalock-Taussig-Thomas shunt.
Also of interest to our readers, to answer their queries – our journals indexing procedure in SCOPUS is in progress, and soon all back issues will be indexed and we will obtain our journal performance metrics, quartile and ranking in SCOPUS journals list. For now, you can find your articles published in our journal after 2017, by searching your name in SCOPUS database. We have reasonable number of citations in SCOPUS, but the whole picture where do we stand and metrics will appear after indexing of all issues as our articles published in back issue have citations as well. Based on current number of citations in SCOPUS for 179 indexed articles (2018-2022) we have 47 citations Hirsch index is 3 (Fig. 1), Crossref/CrossCite – we have 65 citations in journals indexed in Crossref, Google Scholar – 106 citations for all indexed articles our journal`s 5-year Hirsch 5 index (H5) is 4 (Fig. 2). ![]()
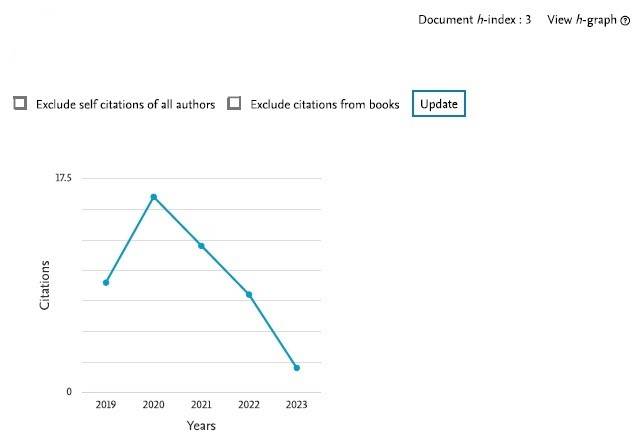
Figure 1. Citations and H-index of the journal for 179 currently indexed articles (2018-2022) in SCOPUS database
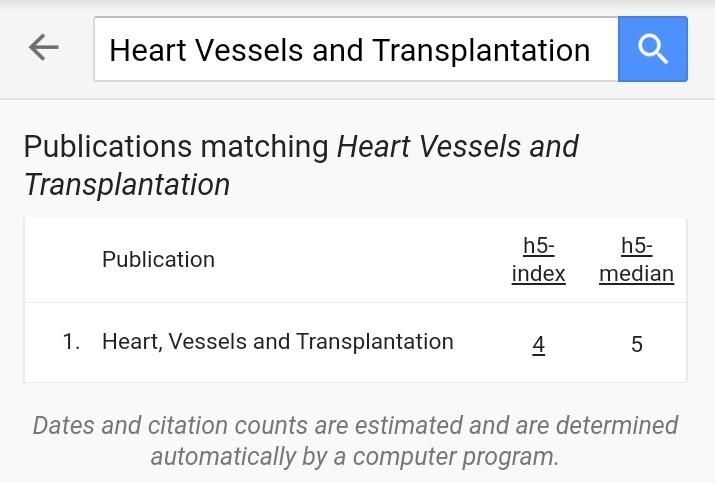
Figure 2. 5-year Hirsch index of the journal in Google Academic (Google Scholar) database
We all have to work together tirelessly to improve it and make a goal to enter higher ranking –authors by submitting quality articles and carefully revising manuscripts according to recommendations of reviewers and editors that are considered eligible for publication by our expert reviewers and editors as we are all participants of peer-review process- `pearl` of evidence –based science and medicine. We will continue our work on our inclusion in other major databases as PUBMED, PMC and Clarivate.
Few updates on trials and guidelines (1-15)- at ACC/WCC 2023, ESC EAPCI,ESC EHRA and HRS congresses, new exciting trials and documents were brought to our attention: ACC documents on management of amyloidosis and heart failure with preserved ejection fractions (HFpEF), ESC EAPCI on use of coronary physiology in stenting and recommendation on coronary artery disease (CAD) management in patients undergoing transcatheter aortic valve replacement (TAVI), ESC EHRA documents on conduction system pacing and arrhythmias in frailty, HRS document on arrhythmias in pregnancy and circulatory support from ISHLT.
International Society for Heart and Lung Transplantation released guideline for mechanical circulatory support, a comprehensive document on use of left ventricular assist and other devices; our editors will introduce it to you in Editorial (13). Documents presented at ACC2023 meeting - one is already introduced in current issue and comment on another (1) will be published soon.
I would like to share news on few trials that attracted my attention at ACC/WCC2023 and HRS 2023 congresses. CLEAR Outcomes trial evaluated bempedoic acid`s, an ATP lyase inhibitor, efficacy in lowering low- density lipoprotein (LDL) cholesterol in statin intolerant patients. Bempedoic acid reduced by 13% (HR 0.87 95%CI – 0.79-0.96, p=0.004) MACE: composite outcome of cardiovascular death, nonfatal myocardial infarction and nonfatal stroke or coronary revascularization as compared to placebo. The therapy was associated with small increase in incidence of gout and cholelithiasis (2). It is an important trial that gives a good alternative for patients intolerant to statins (we encounter such cases) to treat high LDL levels.
TRILUMINATE trial evaluated transcatheter edge-to-edge repair (TEER) of tricuspid valve in patients with severe tricuspid regurgitation. At 30 days primary endpoint (composite of death from any cause or tricuspid-valve surgery, hospitalizations for heart failure) was in favor for TEER group - win ratio was 1.48 (95% CI 1.06-2.13, p=0.02). Patients who underwent TEER had better quality of life and 98% had minimal tricuspid regurgitation as compared to 8.7% in control group. Trial demonstrated that tricuspid valve TEER is safe, reduces markedly severe regurgitation and improves quality of life (3).
RAPID –HF trial evaluated rate –adaptive pacing in patients w ith HFpEF with chronotropic incompetence during exercise demonstrated no benefit in improvement of exercise performance or quality of life (4), thus other means to treat chronotropic incompetence in HFpEF patients should be pursued. Another trial showed that treat-to- target tailoring dose strategy with statins was not inferior to high -dose statin therapy to lower LDL cholesterol to 50-70 mg/dl –MACE at 3-year follow- up was 8.1% in target therapy and 8.7% in high-dose strategy (5). Both tactics may be used.
The interesting trial was presented at HRS 2023 meeting – on efficacy of dual -chamber leadless pacemaker: the goal of sustained atrioventricular synchrony of at least 70% at 3-months by atrial and ventricular pacing was achieved in 97.3% of patients, primary safety and performance end-points were reached in 90% of patients. Thus leadless pacemaker is safe and provides reliable atrioventricular synchrony (9) . We look forward for more such studies as such device allows avoiding lead- related complications that we face in practice.
For management of patients with CAD pre- and post -TAVI, I would like to highlight few points: invasive coronary angiography remains to be main method of coronary anatomy evaluation and computed tomography coronary angiography (CTCA) should be thought in young patients with low cardiovascular risk profile. Management of CAD using percutaneous coronary intervention (PCI) pre-TAVI should be reserved to patients with severe coronary stenosis >70% only in proximal segment and >50 in left main coronary artery particularly presenting with acute coronary syndrome or angina with sub-occlusive lesion >90%; timing depends on presentation and anatomy. For the post- TAVI PCI the THV and implantation technique aimed at preserving of easy coronary access should be considered (6). EAPCI document on use of coronary physiology to guide PCI and stenting, provides expert opinion how to use longitudinal vessel analysis and functional flow physiological measurement to guide stenting (7). We will introduce both documents in relevant Editorial in upcoming issue.
ESC HFA released document on management of acute heart failure patients on pre-discharge and post-discharge stages (8): it provides guidance on clinical and functional assessment of patients pre-discharge – prognostic markers laboratory markers, imaging – including details not only on echocardiography indexes and parameters of filling pressures, but also how to use inferior vena cava imaging and lung ultrasound in assessment of systemic and pulmonary congestion; how to tailor GDMT including comprehensive treatment (ACEI/ARB, ARNI, beta-blockers or MRA, sodium glucose co-transporter inhibitors (SGLT), of note 89% of patients with acute heart failure are not prescribed ARNI) pre- and post-discharge. You can find also recommendations for treatment of comorbidities, rehabilitation on each stage, tele-monitoring and information on use of novel pulmonary artery pressure monitoring devices, and counseling (8).
The consensus statement of arrhythmias in pregnancy was presented at HRS 2023 meeting (10). The document indeed is of particular interest for practicing cardiologists who face such cases in their practice, providing consultations to such patients. The main take home messages are: care of patients should be provided by multidisciplinary team involving cardiologists, maternal fetal care specialists, electrophysiologists, pediatric electrophysiologists, neonatologists, anesthesiologists; the most common arrhythmias are sinus arrhythmia and supraventricular arrhythmias, while life-threatening ventricular and supraventricular are rare arrhythmias, atrial fibrillation is detected more often; the selection of rhythm or rate control should be based on fetus and maternal safety considerations; any invasive procedure should involve reduced radiation time and antiarrhythmic therapy should be selected with less side effects for fetus and mother; cardioversion, EP and ablation procedures, implantation of devices for hemodynamically unstable or life-threatening arrhythmias should be performed with less radiation exposure with fetal monitoring and complex procedure should be sought in experienced centers with protection of fetus from radiation exposure covering maternal abdomen with apron in proning position and left lateral tilt position to avoid aorto-caval compression in third trimester; fetal arrhythmias should be managed by direct intramuscular injections or intraperitoneal injections in fetal hydrops or maternal systemic injections can be used; antiarrhythmic therapy for mothers during pregnancy and postpartum should be selected with less harm for fetus or postpartum during breast-feeding, genetic counseling is recommended for diagnosis of arrhythmias.
At ESC EHRA 2023 congress – arrhythmias management in frail patients (11), and update on conduction system pacing (12) were presented. These two and ACC document on management of HFpEF (1) will be introduced in Editorials by our invited experts and editors.
I recommend also to study the drug-induced arrhythmias AHA scientific statement that provides easy to comprehend knowledge on drugs that cause or exacerbate arrhythmias and their management: bradycardia or atrioventricular block, atrial fibrillation / atrial flutter, atrial tachycardia, atrioventricular nodal reentrant tachycardia, monomorphic ventricular tachycardia, Brugada syndrome, Torsades de Points polymorphic tachycardia an QT interval prolonging drugs (14).
COVID-19 pandemics public health emergency is officially ended by mid-May, 2023 as announced by WHO and CDC (15, 16). however new variants emerge and there are still new cases, so both agencies urge to continue work on vaccinations, stay updated on prevention, on measures what to do if were you in contact or developed disease as well as knowledge for healthcare professionals. Now as CDC recommends vaccination naïve individuals can receive directly 1 bivalent mRNA vaccine as bivalent vaccines reduce significantly hospitalizations, severe disease - intensive care admissions and death (17).
Of course, long COVID is emerging issue affecting different systems like neurological, cardiovascular that we will continue to read and apply the latest recommendations in practice (18). Interestingly, latest knowledge showed that COVID antivirals paxlovid and molnupiravir have been found to reduce the cases with long COVID or PASC - nirmaltrevir reduced PASC by 26% (19).
We will continue to work hard to select and present you the best research, critical assessment of comprehensive evidence, clinical case report articles that can form the basis for future trials or share management of difficult case and articles for continuous medical education and update on clinical practice recommendation.
![]()
Gulmira Kudaiberdieva
Editor-in-Chief
Heart, Vessels and Transplantation
Peer-review: Internal
Conflict of interest: None to declare
Authorship: G.K.
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

