A rare case series of mechanical prosthetic heart valve structural deterioration presented as severe mitral regurgitation
ORIGINAL RESEARCH ARTICLE
A rare case series of mechanical prosthetic heart valve structural deterioration presented as severe mitral regurgitation
Article Summary
- DOI: 10.24969/hvt.2023.396
- Page(s): 278-281
- CARDIOVASCULAR DISEASES
- Published: 16/06/2023
- Received: 13/04/2023
- Revised: 06/06/2023
- Accepted: 06/06/2023
- Views: 6636
- Downloads: 4004
- Keywords: TTK Chitra mechanical valve, structural deterioration of prosthetic heart valve
Address for Correspondence*: Jignesh Kothari, Department of Cardiovascular and Thoracic Surgery, U.N. Mehta Institute of Cardiology and Research Center, Civil Hospital Campus, Asarwa, Ahmedabad-380016, Gujarat, India
Email: jvks20@yahoo.com Mobile: +91-9825845972 Fax: +91-079-22682092
Jignesh Kothari*, Sandip Lukhi, Utkarsh Sanghavi, Devvrat Desai, Ishan Gohil
Department of Cardiovascular and Thoracic Surgery, U.N. Mehta Institute of Cardiology and Research Center, Civil Hospital Campus, Asarwa, Ahmedabad, Gujarat, India
Abstract
Objective: Structural valve deterioration in the form of stenosis or regurgitation or both though being a rare complication with newer generation mechanical heart valves can occur and can be critical.
Case presentation: We report two cases of severe mitral regurgitation due to structural deterioration of TTK Chitra mechanical heart valve (disc fracture) in mitral position.
Conclusion: In patients with mechanical heart valve prosthesis who present with acute decompensated heart failure or congestive heart failure, structural valve deterioration should be suspected and early diagnosis and treatment is the key to success in structural valvular deterioration.
Key words: TTK Chitra mechanical valve, structural deterioration of prosthetic heart valve
Introduction
The introduction of valve replacement surgery in the early 1960s has dramatically improved the outcome of patients with valvular heart disease. Despite the marked improvements in prosthetic valve design and surgical procedures over the past decades, valve replacement does not provide a definitive cure to the patient. Instead, native valve disease is traded for “prosthetic valve disease,” and prosthetic valve hemodynamics, durability and thrombogenicity affect the outcome of patients undergoing valve replacement (1).
Prosthetic heart valve is of two types: 1) Mechanical heart valve, 2) Tissue heart valve.
History and complications of mechanical heart valves
The first mechanical valve was implanted by Dr. Charles Hufnagel in descending thoracic aorta in 1952 which was a ball in cage valve. The Starr-Edwards ball valve was first implanted in 1960 in mitral position. The first tilting disc valve implanted was Bjork-Shiley valve in 1969. The first bileaflet mechanical valve implanted was Gott-Daggett valve in 1963. TTK Chitra mechanical tilting disc valve was first implanted in 1990.
Degenerative calcification, fibrosis, tear or infection are more common in tissue heart valve. Infection, thrombosis, or pannus growth causes non-structural valve failure in mechanical heart valve. The incidence of structural valve dysfunction in mechanical valve caused by material wear and tear is very rare. Björk-Shiley convexo-concave valves have had a high incidence of structural dysfunction. Ball fracture and cloth wear and tear have been reported with Starr-Edwards ball and cage valve. Chitra heart valve prosthesis (CHVP), a tilting disc valve developed in India, is being implanted since 1990 and had very less incidence of structural deterioration.
We report 2 cases of structural deterioration in the form of disc fracture in TTK Chitra heart valve in mitral position.
Case report 1
A 40 years old male presented with dyspnea New York Heart Association (NYHA) class IV in July 2022 having past history of mitral valve replacement (MVR) using 29 mm TTK Chitra prosthetic heart valve in January 2010 for rheumatic heart disease (RHD) with mitral valve (MV) stenosis. After MVR annual echocardiography was done at subsequent follow-up, which showed normal prosthetic valve function. Since January 2022 he had complaint of dyspnea NYHA class II, which gradually progressed to class III since 6 months. In July 2022 he was admitted to the hospital with signs of congestive heart failure (HF).
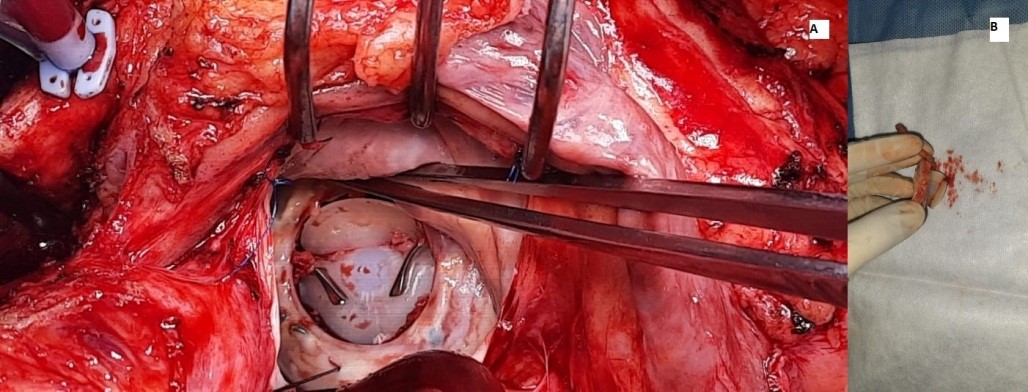
A) B)
Figure 1. Case 1. A) Photograph with in situ TTK CHITRA valve with disc fracture B) Photograph of explanted TTK CHITRA valve in case 1
On auscultation, prosthetic valve click was audible, grade 4/6 pan-systolic murmur over mitral area and basal crepitations were present.Two-dimensional transthoracic echocardiography (2d Echo) showed severe transvalvular mitral regurgitation (MR) (ratio of MV inflow velocity time integral (VTi) and left ventricular outflow tract (LVOT) VTi of 1.68 and the jet occupying almost full of left atrium and hitting the roof of left atrium) and pannus formation with restricted leaflet movement with left ventricular ejection of 40%. Transesophageal echocardiography was done, which was suggestive of the same findings.
Therefore, he was planned for redo MVR after informed consent was obtained. After uneventful redo sternotomy, cardiopulmonary bypass was established. Left atrium was opened and prosthetic MV was assessed. There was transverse disc fracture which caused severe valvular mitral regurgitation (Fig. 1). The valve was explanted in toto and examined. Although the disc was fractured, no part of the disc was missing. A new 29 mm St Jude’s Medical mechanical valve reimplanted. Postoperative recovery was good. He is asymptomatic at 6 months follow up, had started his routine activities after 2.3 months of surgery and 2D echo showed normal prosthetic valve function with normal biventricular function.
Case report 2
A 50 years old male presented with dyspnea NYHA class III in May 2022 having past history of mitral and aortic valve replacement both using TTK Chitra prosthetic heart valve in 2012 for RHD. After surgery annual echo were done at subsequent follow-up which showed normal prosthetic valve function. Since March 2022 he had complaint of dyspnea NYHA class II, which had gradually progressed to NYHA class III since past 3 months.
In May 2022 he was admitted with features of congestive HF. On auscultation, prosthetic valve click was audible, grade 3/6 pan-systolic murmur over mitral area and basal crepitations were present. Transthoracic 2D echo showed severe transvalvular MR due to restricted leaflet movement with left ventricular ejection fraction of 35-40%. Transesophageal echocardiography (TEE) was done, suggestive of severe transvalvular MR (ratio of MV inflow VTi and LVOT VTi of 1.72 and the jet occupying almost entire left atrium and hitting the roof of left atrium) suspecting valvular dehiscence or stuck leaflet in open position, thus he was planned for redo MVR after informed consent was obtained.
After uneventful redo sternotomy cardiopulmonary bypass was established. Left atrium was opened and prosthetic MV mitral valve was assessed, which showed central hole in disc that caused severe valvular MR (Fig. 2). Valve was explanted in toto. Redo MVR was done using 27 mm St Jude’s Medical mechanical valve. Postoperative course was uneventful and he was discharged with stable hemodynamics. He had started his routine activities 3 months after surgery. He is asymptomatic at 6 months follow up and 2d echo showed normal valve function with normal biventricular function.
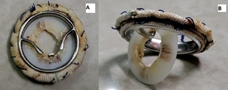
Figure2. Case 2 (A) & (B) - photograph of explanted TTK CHITRA valve with a hole in the center of the disc
Discussion
Valve replacement introduces a new disease process with prosthetic valve-related complications and is not a curative procedure. Structural valve deterioration (SVD) in the form of stenosis, regurgitation or a combination of both is clinically important long-term complication (2). In literature, the incidence of SVD is 0.1–6.0% per patient year and 10–16 years is the mean interval between the initial valve replacement and reoperation (3).
Structural valve deterioration is of two types: 1) Endogenous and 2) Exogenous (3).
Endogenous are caused by valve damage or defect like strut fracture, leaflet escape, occluder dysfunction caused by lipid adsorption (1). Now it has become extremely rare with the improvement of valve design, materials, manufacture, and detection methods in vitro. Exogenous causes include thrombosis, excessive pannus overgrowth into the prosthetic rim, residual chordae tendineae stuck in the prosthetic sewing ring, extremely long residual papillary muscles in left ventricle or calcified tissues under the prosthesis hampering leaflet mobility, excessively long knot end, inappropriate selection of prosthesis or technical issues. Thrombosis and pannus overgrowth are the most common causes of SVD (3).
Mechanical prosthetic valve regurgitation due to SVD is of two types: 1) intra-valvular or 2) para-valvular. Intra-valvular regurgitation can be either immediate or delayed. Immediate regurgitation is due to incomplete disc closure, as a result of sub-valvular chordae or suture hindering the occluder. However, delayed regurgitation is due to restricted leaflet movement because of thrombus or pannus. Infective endocarditis can also cause delayed intra-valvular regurgitation. ‘Washing jets’ are different which prevents stagnation of blood or clot formation on the disc and struts of the valve (4).
Material wear and tear is the cause for structural damage of valve. It may be due to (a) disc dislodgement, (b) disc fracture or (c) strut fracture (d) wear and tear of sewing ring and housing of the mechanical valve. When mechanical damage to the implanted valve occurs, it causes several complications including risk to life. Bjork-Shiley convexo-concave valve model had several incidences of transverse disc fracture and strut fracture leading to embolism and hence was removed from the market in 1986 (5, 6). Presentation is varying from no symptoms to cardiac failure and even with sudden cardiac arrest.
The exact mechanism and cause of structural deterioration are often difficult to identify, but may be thrombus versus pannus or intra- versus para-valvular regurgitation.
Factors responsible for structural valve deterioration include:
1. The pressure difference in the blood flow causes unstable air bubble formation, releases energy on collapsing (high frequency pressure fluctuations) leading to the formation of microcracks in the disc - cavitation (7).
2. Sewing ring compliance is not adequate which causes reduced shock absorption as the leaflet moves.
3. Expired prosthetic valve.
4. Manufacturing defect of prosthetic valve.
5. Surgical mishandling during implantation
TTK Chitra, a mono leaflet valve has housing made up of Haynes-25 alloy (cobalt-nickel-chromium-tungsten alloy), ultra-high molecular weight (UHMW) polyethylene rotatable disc occluder and a sewing ring made up of polyester. In our cases, the patients had been on regular follow-up. 2D echo were done at regular intervals during their follow –ups, which showed normal prosthetic valve—both structurally and functionally. However, both patients presented with features of chronic HF and were diagnosed to have severe intra-valvular regurgitation after 10-12 years of prosthetic valve replacement. Initial suspicion was in favour of thrombus or pannus due to restricted leaflets movement.
The UHMW polyethylene disc rotates on its own axis, and is also able to slide in its plane, thus distributing the stress all over the plane while its movement8. We are unable to explain the mechanism which caused the disc fracture in our cases. We presume that there must have been some thrombus impairing the rotation of the disc on its axis, which in turn led to disc fracture; however, this presumption was not evident on examination of the valve. Another possibility is of manufacturing defect. Fracture of the leaflet is a dreaded complication as the fractured bit can migrate into the systemic circulation.
Conclusion
Structural deterioration of mechanical heart valves is a reported problem with the older generation of mechanical heart valves. Though, being a very rare problem it is still possible with the current generation of mechanical heart valves. In a patient with a mechanical heart valve prosthesis, who presents with acute decompensation or acute onset of symptoms of congestive heart failure, the serious complication of structural valve deterioration must be suspected. Early diagnosis and appropriate treatment in such cases is the key to success.
Ethics: Informed consent was obtained from patients before all procedures.
Peer-review: External and internal
Conflicts of interest: None to declare
Authorship: J.K., S.L., U.S., D.D., I.M. equally contributed to study and manuscript preparation.
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

