A safe single stage strategy for surgical repair of redo coarctation of aorta with coronary artery bypass grafting in adults: A case report
CASE REPORT
A safe single stage strategy for surgical repair of redo coarctation of aorta with coronary artery bypass grafting in adults: A case report
Article Summary
- DOI: 10.24969/hvt.2023.431
- CARDIOVASCULAR DISEASES
- Published: 03/11/2023
- Received: 18/09/2023
- Revised: 13/10/2023
- Accepted: 14/10/2023
- Views: 4602
- Downloads: 3578
- Keywords: : coarctation of aorta, coronary artery bypass surgery, single stage surgery, surgery operative procedures
Address for Correspondence: Jignesh Kothari, Department of Cardio Vascular and Thoracic Surgery U. N. Mehta Institute of Cardiology and Research Center, Civil Hospital Campus, Asarwa, Ahmedabad, Gujarat, 380016, India
Email: jvks20@yahoo.com Phone: +93 9825845972, Fax: +93-079-22682092
Jignesh Kothari: ORCID 0000-0002-7693-2037, Thakut Gowtham: ORCID 0000-0002-1284-8872, Utkarsh Sanghavi: ORCID 0000-0001-8757-7125, Ishan Gohil: ORCID 0000-0002-0573-1211, Devvrat Desai: ORCID 0000-0001-7083-9985
Jignesh Kothari – ORCID: 0000-0002-7693-2037 Utkarsh Sanghavi – ORCID: 0000-0001-8757-7125
Thakut Gowtham, Utkarsh Sanghavi, Ishan Gohil, Devvrat Desai, Jignesh Kothari*
Department of Cardiovascular & Thoracic Surgery, U. N. Mehta Institute of Cardiology and Research Center, Civil Hospital Campus, Asarwa, Ahmedabad, Gujarat, India
Abstract
Objective: The association of coarctation of aorta (CoA) and coronary artery disease is rare. To formulate single stage safe strategy for redo repair of aortic coarctation and simultaneous coronary artery bypass grafting (CABG).
Case presentation: The present case report describes a 55-year-old male, who underwent a redo safe single -stage surgical repair for both pathologies. CoA was tackled by ventral aortic repair followed by coronary artery bypass grafting under cardiopulmonary bypass. The vascular prosthesis was anastomosed to descending thoracic aorta in end-to- side fashion, and it was located posterior to the inferior vena cava through the oblique sinus but inferior to the superior vena cava and curved around the right atrium, anastomosed to ascending aorta.
Conclusion: Ventral aortic repair through a midline approach is our preferred technique for redo surgical repair of CoA. Dual arterial cannulation ensures adequate perfusion of both upper and lower extremities.
Key words: coarctation of aorta, coronary artery bypass surgery, single stage surgery, surgery operative procedures
Introduction
Coarctation of the aorta (CoA) occurs in approximately 4 of 10,000 live births and comprises 5% to 8% of congenital heart disease (1). Because of its long-term tolerance, CoA in adults is associated with a high level of collateral circulation and vascular variation. The association of aortic coarctation with coronary artery disease is not rare in patients past 35 years of age (2). Few patients with aortic coarctation become symptomatic at 30–40 years of age when the occurrence of coronary artery disease increases. Surgical management becomes difficult particularly when both the pathologies coexist. Usually a median sternotomy and repair of coarctation using a long vascular prosthesis, which is connected to the descending thoracic or abdominal aorta or iliac artery is preferred (3-5).
In this report, we describe our experience of redo repair of aortic coarctation and simultaneous coronary artery bypass grafting (CABG) using single-stage surgical technique with good outcomes.
Case report
A 55-year-old male presented to our hospital with headache, chest tightness, dyspnea, palpitations on exertion. He had been categorized as NYHA class IV since 4 to 5 months and had history of claudication pain in both lower limbs. He had a prior history of CoA repair using a graft between left subclavian artery to descending thoracic aorta in 2008 via left posterolateral thoracotomy.
Echocardiography showed normal left ventricular ejection fraction (LVEF) with mild aortic, and mitral valve regurgitation and concentric left ventricular hypertrophy (LVH). Computed tomography angiography (CTA) and 3D CT scan reconstruction revealed post ductal CoA with multiple enlarged collaterals in mediastinum, paravertebral region, bilateral internal mammary arteries and absence of contrast filling within the graft suggesting graft occlusion between left subclavian artery and descending thoracic aorta (Fig. 1). Coronary angiography revealed >90% stenosis in the left anterior descending (LAD) artery and proximal right coronary artery - 90%. After discussing with interventional cardiologist and radiologist, decision was taken to perform redo surgery.
![]()
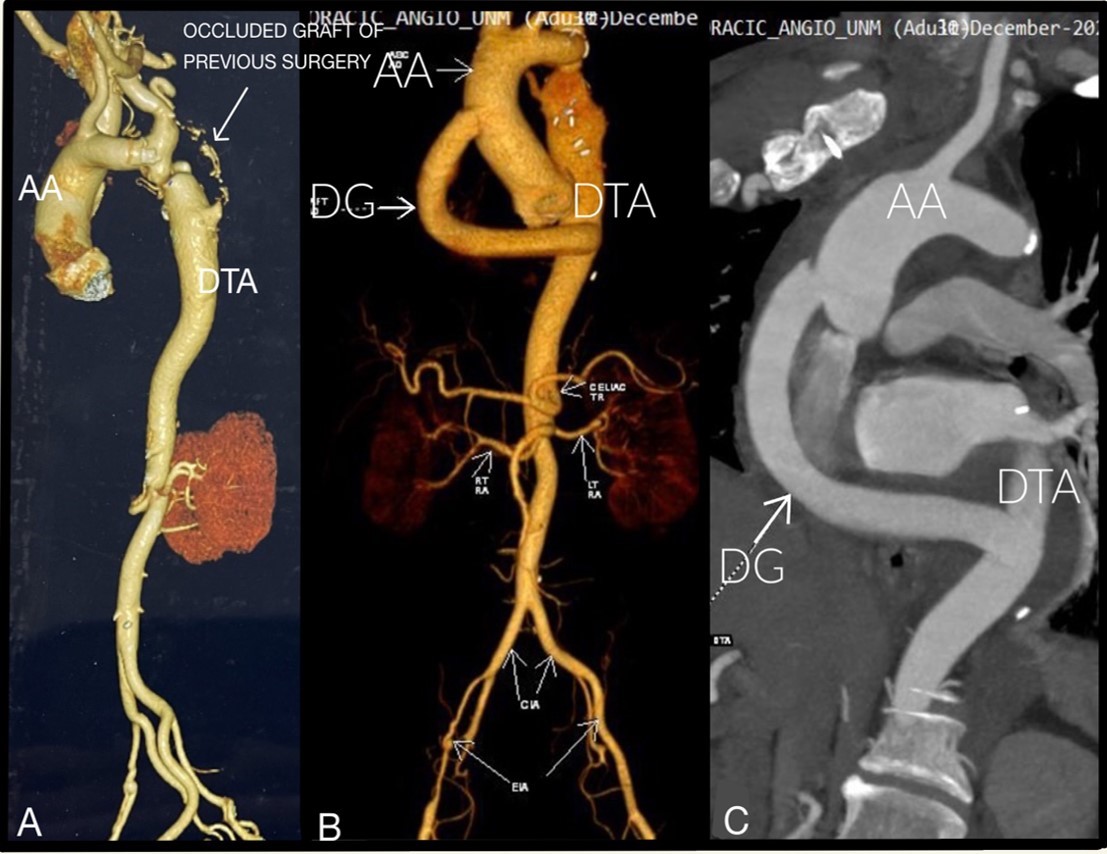
Figure 1. A) Preoperative CTA showing CoA, with occluded graft between left subclavian artery and descending thoracic aorta; B) and C) Postoperative CTA showing patent dacron graft from ascending aorta to descending thoracic aorta
AA- ascending aorta, CoA- coarctation of aorta, CTA – computed tomography angiography, DG- Dacron graft, DTA- descending thoracic aorta
Operative technique
After written, informed consent was obtained from patient, we performed ascending-to-descending aortic bypass, CoA repair, and CABG. Right radial and left femoral arterial lines were secured. The surgical approach involved a median sternotomy. Cardiopulmonary bypass was established between the right common femoral artery, the right axillary artery done by end-to-side anastomosis of 6mm polytetrafluoroethylene (PTFE) graft to maintain perfusion to both upper and lower half of the body, and the superior and inferior vena cava (Fig. 2). Left interior mammary artery (LIMA) was harvested. Antegrade root cold cardioplegia was given. Following the diastolic arrest of heart, the apex was elevated out of the pericardial wall to expose the posterior pericardium. A longitudinal posterior pericardial incision over the descending aorta was made, which allowed for exposure of the anastomotic stoma. A sidewall vascular clamp was used to control the descending aorta, and end-to-side anastomosis of a 16 mm Dacron graft to the descending aorta was deployed by a continuous 5-0 polypropylene suture. The graft was passed posterior to the inferior vena cava, anterior to right inferior pulmonary vein through the oblique sinus but inferior to the superior vena cava and curved around the right atrium (Fig. 3A). During graft suturing, moderate hypothermic circulatory arrest (28°C) was achieved. The proximal anastomosis of the graft to aorta was done using 5-0 Prolene using sidewall vascular clamp. CABG was performed with the LIMA to LAD. The operation time was 220 min, the cardiopulmonary bypass time was 110 min, and the cross-clamp time was 60 min.
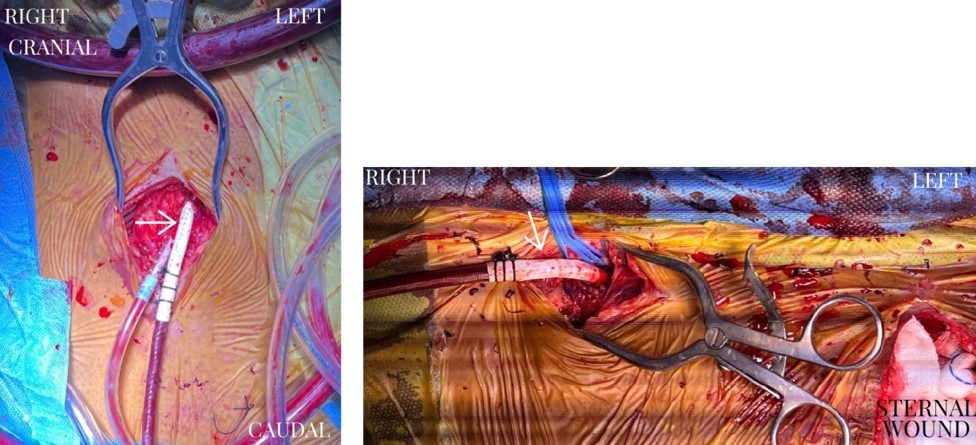
Figure 2. A) Intraoperative picture illustrating right femoral arterial cannulation using PTFE graft B) intraoperative picture illustrating right axillary arterial cannulation using PTFE graft
PTFE – polytetrafluoroethylene
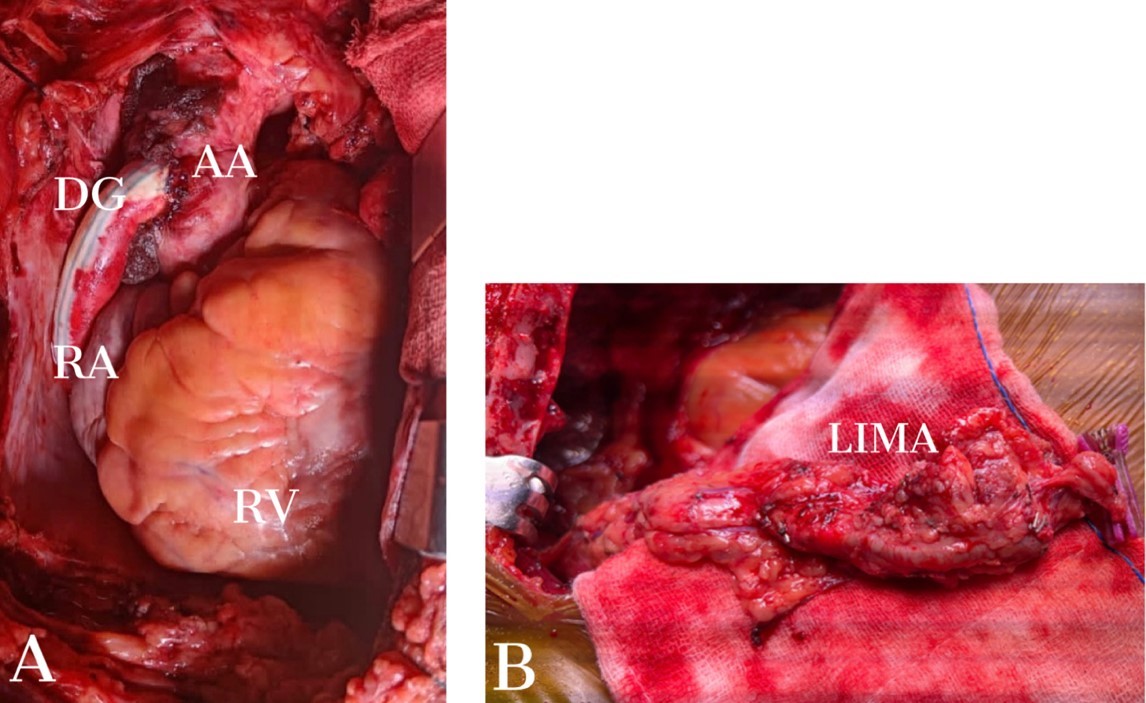
Figure 3. A) Intraoperative picture showing anastomosis of Dacron graft between ascending aorta and descending thoracic aorta B) Intraoperative picture of hypertrophied LIMA
AA – ascending aorta, DG – Dacron graft, LIMA - left internal mammary artery, RA- right atrium, RV – right ventricle
The right coronary artery was not re-vascularized as it was very small in caliber (<1mm).
The patient had 3 days of intensive care unit stay, and was discharged on day 8. Post-operative 3D CT scan reconstruction revealed good flow from ascending to descending aorta with no leak and flowing LIMA to LAD (Fig. 4). At 6-months follow-up, patient was in NYHA class II with stable hemodynamics.
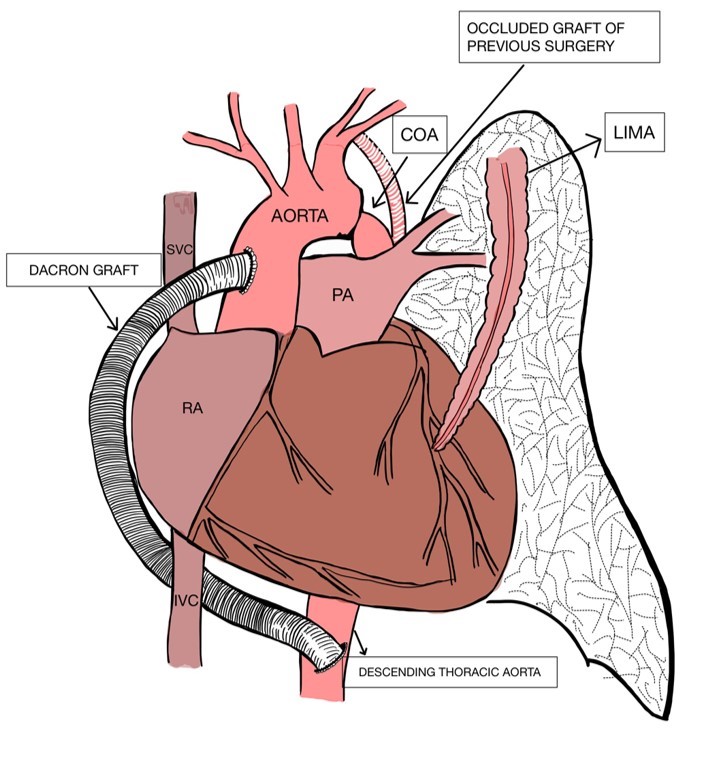
Figure 4. Diagrammatic representation of ventral aortic repair for CoA and LIMA to LAD grafting
CoA- coarctation of aorta, LAD – left anterior descending artery, LIMA- left internal mammary artery
Discussion
The simultaneous correction of ischemic heart disease and CoA requires two different stages of operation. Correction of the coarctation alone is associated with increased perioperative myocardial infarction (6). On the other hand, correction of the cardiac lesion alone is associated with increased postoperative renal failure and paraplegia as a result of inadequate distal organ perfusion (7). The association of CoA with coronary artery disease is common in patients after 4th decade of life due to bimodal presentation (2). Patients with severe CoA are either treated in infancy and/or childhood or die during childhood without treatment. The majority of CoA patients who survive to adulthood develop compensatory collateral circulation. Surgical difficulties are likely for elderly patients with CoA and other cardiovascular diseases due these collaterals.
Cannulation technique which we had used in our case is preferred, so as to secure sufficient cerebral protection and to maintain perfusion to lower extremity (Fig. 2). It is difficult to direct the graft around the right margin of the heart without compressing the right atrium or right ventricle. This is very well done by directing the graft behind the inferior vena cava and anterior to the right inferior pulmonary vein but inferior to superior vena cava in the oblique sinus. This course also ensures that the graft remains in a posterior location and to the right side of the sternum, which can reduce the complications of redo sternotomy less.
We used the hypertrophied internal mammary artery for coronary grafting because the difference in luminal diameters did not preclude the procedure. We have not found any reference concerning the use of the hypertrophied internal mammary artery as a coronary graft. Internal mammary artery dissection, identification of its intercostal branches and the placement of ligatures or clips offers no difficulties. This was a macroscopically healthy artery, with 3 mm caliber, and no atheromatous plaques nor clarification with good flow.
Conclusion
Ventral aortic repair through a midline approach is our preferred technique for redo surgical repair of this entity, because it avoids the extensive network of collateral vessels on the chest wall, enables simultaneous treatment of associated lesions as in our case with CABG, and in all likelihood reduces morbidity and mortality. Dual arterial cannulation ensures perfusion of both extremities. It also avoids or minimizes the risk of paraplegia, and avoids the need for an additional surgical sternotomy or thoracotomy with a staged procedure.
Ethics: Informed consent was obtained from patient before all procedures. The patient consented to the submission and publication of this report.
As per our Institute protocol, we do not have to approve the image and case
report before publication.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: T.G., U.S., I.G., D.D., and J.K. equally contributed to case management and preparation of manuscript
Acknowledgment and funding: None to declare
References
- 1.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002; 39: 1890–900.
- 2.Cohen M, Fuster V, Steele PM, Driscoll D, McGoon DC. Coarctation of the aorta. Long-term follow-up and prediction of outcome after surgical correction. Circulation 1989; 80: 840–5.
- 3.Fernandez de Caleya D, Duarte J, Eguren A, Torrente N, Lozarro A, Nuche J. Combined therapy of coarctation and coronary artery dis- ease in an adult. Thorac Cardiovasc Surg 1993; 41: 127–9.
- 4.Bartoccioni S, Giombolini C, Fiaschini P, Martinelli G, Fedeli C, Di Lazzaro D, et al. Aortic coarctation, aortic valvular stenosis, and coronary artery disease: combined one-stage surgical therapy operation. J Card Surg 1995; 10: 594–6.
- 5.Thomka I, Szedo F, Arvay A. Repair of coarctation of the aorta in adults with simultaneous aortic valve replacement and coronary artery bypass grafting. Thorac Cardiovasc Surg 1997; 45: 93–6.
- 6.Pethig K, Wahlers T, Tager S, Borst FG: Perioperative complica tions in combined aortic valve replacement and extraana-tomic ascending-descending bypass. Ann Thorac Surg 1996, 61: 1724-6.
- 7.Brewer LA, Fosburg RG, Mulder GA, Verska JJ. Spinal cord complications following surgery for coarctation of the aorta: a study of 66 cases. J Thorac Cardiovasc Surg 1972, 64: 368-81.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

