Attitude to evidence-based practice amongst international thoracic surgeons: preliminary observations from a web-based survey
BRIEF REPORT
Attitude to evidence-based practice amongst international thoracic surgeons: preliminary observations from a web-based survey
Article Summary
- DOI: 10.24969/hvt.2025.562
- CARDIOVASCULAR DISEASES
- Published: 18/04/2025
- Received: 01/03/2025
- Revised: 14/04/2025
- Accepted: 15/04/2025
- Views: 2605
- Downloads: 2179
- Keywords: Evidence-based medicine; thoracic surgery; surgical training; survey; medical education
Address for Correspondence: Federico Tacconi, Unit of Thoracic Surgery, Tor Vergata University Polyclinic, Viale Oxford, 81, 00133 Rome, Italy
E-mail: tacconifederico@gmail.com Phone: +3906-20902884 Fax: +3906-20902883
ORCID: Federico Tacconi - 0000-0001-8850-5027; Alexandro Patirelis - 0009-0009-7409-8470; Gianluca Vanni - 0000-0002-3006-5855; Vincenzo Ambrogi - 0000-0002-8947-3175
Alexandro Patirelis1,2, Vincenzo Ambrogi1,2, Sebastiano Angelo Bastone1,2, Gianluca Vanni1, Federico Tacconi1,2*
1Department of Surgery, Tor Vergata University Polyclinic, Viale Oxford 81, 00133, Rome, Italy
Rome, Italy
2Unit of Thoracic Surgery, Tor Vergata University Polyclinic, Viale Oxford 81, 00133, Rome, Italy
Rome, Italy
Abstract
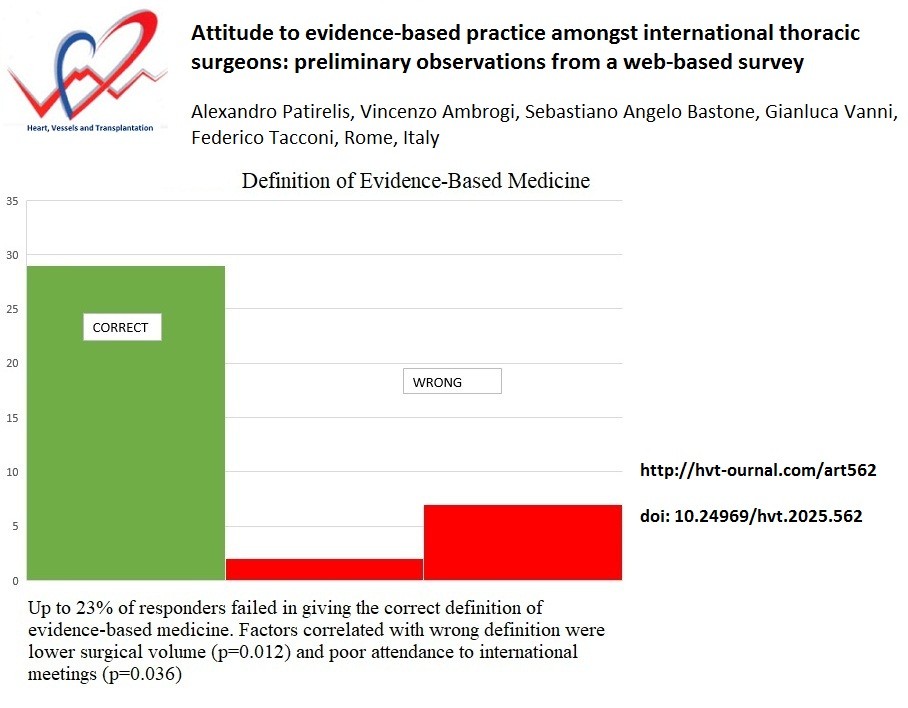
Evidence-based medicine is a process to de-emphasize the role of intuition and anecdotal experiences as a guide to clinical practice. We performed a survey to assess the comprehension and attitude toward evidence-based practice amongst a group of thoracic surgeons. There were 38 responders out of 151 surgeons. Up to 23% of responders failed in giving the correct definition of evidence-based medicine. Factors correlated with wrong definition were lower surgical volume and poor attendance to international meetings. Our survey suggests that more focus on evidence-based medicine concepts should be put during surgical training.
Graphical abstract
Key words: Evidence-based medicine; thoracic surgery; surgical training; survey; medical education
Introduction
Evidence-based medicine (EBM) can be conceptualized as a process to de-emphasize the role of intuition, pathophysiological reasoning, and anecdotal experiences as a guide to clinical practice (1, 2). Since its introduction, adherence to EBM is being fostered by an increasing number of health-care institutions. However, there are still barriers to its complete acceptance (3, 4). One of the main sources of skepticism is the poor awareness of EBM’s basic principles, which - in turn – might generate misconceptions about EBM’s objectives and limitations.
In this cross-sectional survey, we sought to assess the extent of comprehension and attitude toward EBM practice amongst thoracic surgeons.
Methods
Study design – cross-sectional survey
International thoracic surgeons at different job level were reached by either instant messaging application or email. They were provided with link to a 20-item e-questionnaire, and the answers were saved anonymously. The study adhered in many points to the Consensus-Based Checklist for Reporting Survey Studies, as recommended by the EQUATOR Network (5). The only exception was that the questionnaire had no previous validation, as it included well-defined concepts rather than constructs.
There were both single-answer/multiple-choice questions and rating-scale questions. The main survey’s objective was to assess how many responders succeeded at correctly defining EBM as a “practice founded on high-quality clinical studies”. Other questions assessed the time devoted to continuous medical education, the number of attended international meetings, and engagement in quality improvement initiatives. Two questions measured the individual surgical volume, and the preferred surgical approach for lung resections. Two questions assessed how likely the responder was to offer surgery in debatable circumstances, that is, single lung metastasis and upfront left-upper lobectomy for cT1bN2a non-small cell lung cancer. Other questions regarding institutional and government support to EBM practice were not analyzed for the present study. Secondary outcomes were the correlations between correct EBM definition and other variables of interest. To this purpose, the Cramer’s V test was applied after dichotomization into binary categories. A p-level <0.05 was regarded as significant.
Results
There were 38 responders out of 151 surgeons. Table 1 shows general features of survey’s populations and the complete list of questions. About 60% of participants were associate specialists or consultants and about 70% of them were under 50 years old. The majority of them worked in public and academic hospitals (26/38, 68.4%) and revealed that they were asked for mandatory training or updates (24/38, 63.2%). Impressively, up to 23% of responders failed at correctly defining EBM. In particular, 13 % thought that EBM is founded on “traditional medical habits”, while 5% felt that EBM is strictly linked to “bench sciences and laboratory data”.
|
Table 1. Answers to web-based questionnaire |
|
|
Questions |
Answers, n (%) |
|
Age group, years 25-30 31-40 41-50 51-60 >60 |
9 (23.7) 11 (28.9) 10 (26.3) 6 (15.8) 2 (5.3) |
|
Position Associate specialist Consultant Resident/Fellow PGY 1-2 |
8 (21.1) 15 (39.5) 11 (28.9) 4 (10.5) |
|
Definition of EBM A medical practice founded on observations coming from good quality clinical studies (✓) A medical practice founded on well known and consolidated habits, rather than on innovations (X) A medical practice founded on uncontrovertible findings from bench science and laboratory data (X) |
29 (76.3) 2 (5.3) 7 (18.4) |
|
Continues on page XXX |
|
|
Continued from page XXX |
|
|
Table 1. Answers to web-based questionnaire |
|
|
Questions |
Answers, n (%) |
|
International meetings attended per year <2 2-3 3-4 4-5 >5 |
18 (47.4) 18 (47.4) 0 (0.0) 1 (2.6) 1 (2.6) |
|
Periodical revalidation or appraisal of license Yes No |
16 (42.1) 22 (57.9) |
|
Surgical operations per year as first operator <40 41-60 61-80 81-100 >100 |
8 (21.1) 11 (28.9) 8 (21.1) 4 (10.5) 7 (18.4) |
|
Current hospital Public and academic Public and non-academic Private and academic Private and non-academic Mixed/other |
26 (68.4) 5 (13.2) 5 (13.2) 1 (2.6) 1 (2.6) |
|
Mandatory training/updates Yes No |
24 (63.2) 14 (36.8) |
|
Preferred approach for major lung resections Multiportal VATS Uniportal VATS RATS Open Open with limited access |
21 (55.3) 8 (21.1) 1 (2.6) 5 (13.2) 3 (7.9) |
|
Promotion of implementations in current hospital Yes No |
28 (73.7) 10 (26.3) |
|
Field of implementation Surgical technique/device/postop management Communication/team working Relationship with patients and relatives Teaching/training Other |
26 (68.4) 6 (15.8) 1 (2.6) 1 (2.6) 4 (10.5) |
|
Professional time dedicated to refresh guidelines/recommendations <5% 6-10% 11-15% 16-20% >20% |
5 (13.2) 12 (31.6) 10 (26.3) 5 (13.2) 6 (15.8) |
|
Continues on page XXX |
|
|
Continued from page XXX |
|
|
Table 1. Answers to web-based questionnaire |
|
|
Questions |
Answers, n (%) |
|
How would you agree to the following plan: "Offer resection of a single metastasis from colorectal cancer in a 72 year old patient” 1 (no agreement) 2 3 4 5 (strong agreement) |
0 (0.0) 1 (2.6) 8 (21.1) 5 (13.2) 24 (63.2) |
|
How would you agree to the following plan: "Offer upfront left upper lobectomy for cT1b NSCLC with single PET-positive station 5 lymph node" 1 (no agreement) 2 3 4 5 (strong agreement) |
4 (10.5) 4 (10.5) 9 (23.7) 9 (23.7) 12 (31.6) |
|
How would you agree to the following sentence: "Adherence to guidelines should be always pursued whenever possible" 1 (no agreement) 2 3 4 5 (strong agreement) |
1 (2.6) 3 (7.9) 5 (13.2) 18 (47.4) 11 (28.9) |
|
How would you agree to the following sentence: "Adherence to guidelines might jeopardize surgeons' ability to address individual patient’s needs" 1 (no agreement) 2 3 4 5 (strong agreement) |
6 (15.8) 6 (15.8) 14 (36.8) 9 (23.7) 3 (7.9) |
|
How much your hospital is promoting and fostering adherence to guidelines? Not too much A little bit Enough A lot Even too much |
7 (18.4) 5 (13.2) 14 (36.8) 12 (31.6) 0 (0.0) |
|
How much do you think your country is promoting and fostering adherence to guidelines? Not too much A little bit Enough A lot Even too much |
7 (18.4) 6 (15.8) 15 (39.5) 8 (21.1) 2 (5.3) |
|
EBM -evidence-based medicine, PGY - postgraduate training year. RATS - robot-assisted thoracic surgery, VATS - video-assisted thoracic surgery |
|
Amongst factors correlated with wrong EBM definition, there were lower surgical volume (p=0.012), and poor attendance to international meetings (p=0.036).
Interestingly, more than 50% of participants felt that adherence to guidelines can jeopardize at some extent the ability of addressing individual patients’ needs. In addition, about 30-35% of participants revealed that their hospital or country do not promote or foster adherence to guidelines.
Participants who defined EBM properly were more likely to mark multiportal videothoracoscopy as the preferred surgical approach. No other correlation was found (Table 2).
|
Table 2. Correlations between answers and ability to correctly define evidence-based medicine |
||||
|
Variables |
Definition of EBM |
Cramer’s V |
p |
|
|
Correct (n=29) |
Wrong (n=9) |
|||
|
Age, years, n (%) ≤40 ≥41 |
15 (51.7) 14 (48.3) |
5 (55.6) 4 (44.4) |
0.033 |
0.84 |
|
Position, n (%) Associate specialist/Consultant Resident/Fellow/PGY 1-2 |
17 (58.6) 12 (41.4) |
6 (66.7) 3 (33.3) |
0.070 |
0.67 |
|
International meetings per year, n (%) <2 ≥2 |
11 (37.9) 18 (62.1) |
7 (77.8) 2 (22.2) |
0.34 |
0.036 |
|
Periodical revalidation or appraisal of license, n (%) Yes No |
14 (48.3) 15 (51.7) |
2 (22.2) 7 (77.8) |
0.22 |
0.17 |
|
Surgical operations per year as first operator, n (%) ≤60 ≥61 |
12 (41.4) 17 (58.6) |
8 (88.9) 1 (11.1) |
0.31 |
0.012 |
|
Current hospital, n (%) Academic Non-academic |
25 (86.2) 4 (13.8) |
6 (66.7) 3 (33.3) |
0.21 |
0.19 |
|
Mandatory training/updates, n (%) Yes No |
16 (55.2) 13 (44.9) |
8 (88.9) 1 (11.1) |
0.30 |
0.067 |
|
Preferred approach for major lung resections, n (%) Minimally invasive Open |
22 (75.9) 7 (24.1) |
8 (88.9) 1 (11.1) |
0.14 |
0.40 |
|
Promotion of implementations in current hospital, n (%) Yes No |
22 (75.9) 7 (24.1) |
6 (66.7) 3 (33.3) |
0.089 |
0.58 |
|
Field of implementation, n (%) Surgical technique/device/postop management Other |
21 (72.4) 8 (27.6) |
5 (55.6) 4 (44.4) |
0.15 |
0.34 |
|
Professional time dedicated to refresh guidelines/recommendations, n (%) ≤10% ≥11% |
13 (44.8) 16 (55.2) |
4 (44.4) 5 (55.6) |
0.003 |
0.98 |
|
How would you agree to the following plan: "Offer resection of a single metastasis from colorectal cancer in a 72 year old patient”, n (%) 1-3 4-5 |
6 (20.7) 23 (79.3) |
3 (33.3) 6 (66.7) |
0.13 |
0.44 |
|
How would you agree to the following plan: "Offer upfront left upper lobectomy for cT1b NSCLC with single PET-positive station 5 lymph node", n (%) 1-3 4-5 |
13 (44.8) 16 (55.2) |
4 (44.4) 5 (55.6) |
0.003 |
0.98 |
|
Continues on page XXX |
||||
|
Continued from page XXX |
||||
|
Table 2. Correlations between answers and ability to correctly define evidence-based medicine |
||||
|
Variables |
Definition of EBM |
Cramer’s V |
p |
|
|
Correct (n=29) |
Wrong (n=9) |
|||
|
How would you agree to the following sentence: "Adherence to guidelines should be always pursued whenever possible", n (%) 1-3 4-5 |
7 (24.1) 22 (75.9) |
2 (22.2) 7 (77.8) |
0.019 |
0.91 |
|
How would you agree to the following sentence: "Adherence to guidelines might jeopardize surgeons' ability to address individual patient’s needs", n (%) 1-3 4-5 |
20 (69.0) 9 (31.0) |
6 (66.7) 3 (33.3) |
0.021 |
0.90 |
|
How much your hospital is promoting and fostering adherence to guidelines?, n (%) Not too much/ a little bit Enough/ a lot/ even too much |
11 (37.9) 18 (62.1) |
1 (11.1) 8 (88.9) |
0.24 |
0.13 |
|
How much do you think your country is promoting and fostering adherence to guidelines?, n (%) Not too much/ a little bit Enough/ a lot/ even too much |
12 (41.4) 17 (58.6) |
1 (11.1) 8 (88.9) |
0.27 |
0.095 |
|
EBM - evidence-based medicine, PGY - postgraduate training year, RATS - robot-assisted thoracic surgery, VATS - video-assisted thoracic surgery |
||||
Discussion
Despite an EBM approach is currently being encouraged by an increasing number of institutions worldwide, there are still barriers to complete acceptance of it. Reluctance toward EBM is mainly related to intellectual misconceptions of true EBM objectives and limitations. Other factors are poor attitude to welcome changes in daily practice, lack of institutional support, skepticism on reliability of clinical study results, and others (3, 4).
The most interesting result of our survey is that a not negligible percentage of responders failed at marking the correct definition of EBM. In particular, the rate of wrong answer was higher amongst thoracic surgeons with smaller surgical volume and poor attendance to international meetings. This finding might suggest a stronger connection with EBM’s principles amongst surgeons with a stronger proactive attitude. Yet another interesting point was the relationship between correct EBM definition and preference of multiportal videothoracoscopy approach, in lieu of alternatives whose advantages are still uncertain (single-port videothoracoscopy) or destined to obsolescence. This fact might suggest a correlation between evidence-based attitude and more adherence to universally shared surgical standards.
Study limitations
This preliminary study has different limitations to consider. First of all, only 25% of surgeons took part in the survey. This low response rate could limit the generalizability of the results due to possible selection bias (i.e. only surgeons interested in EBM could have answered the survey thus underestimating the results). Another limitation is the lack of validation for the questionnaire, which could not have really captured the attitude of surgeons towards EBM.
Lastly, due to the reduced number of answers, we could not perform additional statistical analysis.
Conclusion
Despite its preliminary nature, our survey suggests that more focus on EBM concepts should be put during surgical training. In this regard, it would be important to debunk the misconception of EBM as a dogmatic body of impersonal protocols. Educational initiatives should highlight that attention to individual patients’ needs is instead a basic concept of EBM itself. Adoption of web-based resources to facilitate surgeons’ access to guidelines and recommendations would also be welcome and might help viewing at EBM as a flexible and supportive tool rather than a sort of professional imprisonment. Further investigations with an externally validated questionnaire involving a wider group of surgeons are warranted to better address these points, and to monitor changes over time.
Ethics: This study does not involve patients nor animal models. We consulted with the Internal Review Board who determined that this study did not need ethical approvalInformed consent was obtained from participants of survey.
Peer-review- External and internal
Conflict of interest- None to declare
Authorship: Conceptualization - F.T.; Methodology: F. T., A.P., G.V.; Formal analysis and investigation - F.T.; A.P.; Writing - original draft preparation: F.T., A. P., G.V.; Writing - review and editing: F.T., V.A.; Supervision: V.A.
Thus, all authors fulfilled all authorship criteria for publication.
Acknowledgement and Funding: None to declare
Statement on A.I.-assisted technologies use- Authors declare that they did not use AI-assisted technologies in preparation of this manuscript
Availability of data and material: All data generated or analyzed during this study are included in this published article
References
| 1.Djulbegovic B, Guyatt GH. Progress in evidence-based medicine: a quarter century on. Lancet 2017; 390: 415-23.doi: 10.1016/S0140-6736(16)31592-6 https://doi.org/10.1016/S0140-6736(16)31592-6 PMid:28215660 |
||||
| 2.Akobeng AK. Principles of evidence based medicine. Arch Dis Child 2005; 90: 837-40. doi: 10.1136/adc.2005.071761 https://doi.org/10.1136/adc.2005.071761 PMid:16040884 PMCid:PMC1720507 |
||||
| 3.Abu-Odah H, Said NB, Nair SC, Allsop MJ, Currow DC, Salah MS, et al. Identifying barriers and facilitators of translating research evidence into clinical practice: a systematic review of reviews. Health Soc Care Community 2022; 0: e3265-76. doi: 10.1111/hsc.13898. 4.Greenhalgh T, Howick J, Maskrey N. Evidence based medicine: a movement in crisis? BMJ 2014; 348: g37255 doi: 10.1136/bmj.g3725 https://doi.org/10.1136/bmj.g3725 PMid:24927763 PMCid:PMC4056639 |
||||
| 5.Sharma A, Duc NTM, Thang TLM, Nam NH, Ng SJ, Abbas KS, et al. A consensus-based checklist for reporting of survey studies (CROSS). J Gen Int Med 2021; 36: 3179-87. doi: 10.1007/s11606-021-06737-1 https://doi.org/10.1007/s11606-021-06737-1 PMid:33886027 PMCid:PMC8481359 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

