Stent grafts implantation in patients with life-threatening aortic conditions – first experience in Kyrgyz Republic
CONFERENCE PAPER
Stent grafts implantation in patients with life-threatening aortic conditions – first experience in Kyrgyz Republic
Article Summary
- DOI: 10.24969/hvt.2019.156
- Page(s): 208-213
- Published: 11/10/2019
- Views: 6500
- Downloads: 5223
- Keywords: thoracic endovascular aortic repair (TEVAR), endovascular aneurism repair (EVAR), life-threatening aortic conditions, aortic aneurysm, aortic dissection, stent graft
Address for Correspondence: Semen Schevgun, International School of Medicine, Bishkek, Kyrgyzstan, Email: schevgun@mail.ru Phone No: +996 550 177 377
International School of Medicine, Bishkek, Kyrgyzstan
Abstract
Objective: Aortic diseases remain an acute and debatable problem. Among all the aortic pathologies, the most dangerous are dynamic aneurysmal expansion, traumatic dissections and / or aneurysms, pure aortic intima dissections. Contemporary and less invasive treatment method is the stent graft implantation into aorta.
This report describes the first experience of thoracic endovascular aortic repair (TEVAR) and endovascular aneurysm repair (EVAR) in the Kyrgyz Republic in consecutive patients with life-threatening aortic conditions.
Methods: Nine patients, who underwent TEVAR and EVAR, were presented after all clinical examinations, echocardiography and computed tomography angiography with various life-threatening aortic diseases. Among the pathologies there were 2 (22.2%) dissections only, traumatic aneurysm 1 (11.1%), aneurysm without dissection 1 (11.1%), aneurysm with intimal dissection 5 (55.6%). Seven patients with dissection had type B (The Stanford classification).
Results: TEVAR was performed in eight cases EVAR just in one. All patients reached the 6-month endpoint. None of the following, such as aneurysm expansion, aneurysm thrombosis or a functioning of false lumen at the sites of the stent graft implantation has been recorded. In addition, no further progression of the false lumen below the implantation zones was visualized. Mean diameter of stent grafts was 31.4(4.8) mm and 188.9(34.6) mm in length.
Conclusion: This modest observation showed the effectiveness of stent grafts implantation procedures in various aortic life-threatening conditions, such as aneurysm and / or aortic intima dissection.
Key words: thoracic endovascular aortic repair (TEVAR), endovascular aneurysm repair (EVAR), life-threatening aortic conditions, aortic aneurysm, aortic dissection, stent graft
Introduction
Aortic diseases remain an acute and debatable problem. Among all the aortic pathologies, the most dangerous are dynamic aneurysmal expansion, traumatic dissections and/or aneurysms, pure aortic intima dissections.
Aortic aneurysms (AAs) are more common in men than in women. Abdominal AA prevalence rates are estimated at 1.3–8.9% in men and 1.0–2.2% in women and are more often located in the infrarenal segment. However, thoracic aortic aneurysms (TAAs) have an estimated incidence of at least 5-10 per 100.000 person-years. According to location, TAAs are classified into aortic root or ascending aortic aneurysms, which are most common (≈60%), followed by aneurysms of the descending aorta (≈35%) and aortic arch (<10%). Aneurysm over time may undergo dissection or rupture (1, 2).
Acute aortic syndrome (AAS) is the modern term that includes aortic dissection, intramural hematoma (IMH), and symptomatic aortic ulcer. In the classic sense, acute aortic dissection requires a tear in the aortic intima that is commonly preceded by medial wall degeneration or cystic media necrosis. Blood passes through the tear separating the intima from the media or adventitia, creating a false lumen. Propagation of the dissection can proceed in anterograde or retrograde fashion from the initial tear involving side branches and causing complications such as malperfusion syndromes, tamponade, or aortic valve insufficiency. By convention, acute disease is distinguished from chronic disease at an arbitrary time point of two weeks from initial clinical presentation (hyperacute: <24 hours, acute: 1 to 14 days, subacute: >14 to 90 days, chronic: >90 days) and is typically manifested with symptoms (3-9).
Patients with AA and dissections undergo open aortic procedures, which often lead to complications and death. Contemporary and less invasive treatment method is the stent graft implantation into aorta. However, this requires certain skills. This report is focused on the first stents grafts implantation experience, in the nine consecutive patients, in Kyrgyzstan.
Methods
Patients were presented after all clinical examinations, echocardiography and computed tomography (CT) angiography with various life-threatening aortic diseases. Among the pathologies there were 2 (22.2%) dissections only, traumatic aneurysm 1 (11.1%), aneurysm without dissection 1 (11.1%), aneurysm with intimal dissection 5 (55.6%). Mean diameter of aneurysms was 6.8 (2.1) cm. Seven patients with dissection had type B (The Stanford classification). Five (55.6%) patients were females. One patient had Marfan syndrome and underwent the David procedure due to type A dissection. After that, type B dissection was detected (The Stanford classification). We reported about it earlier (10). Another patient previously had coronary artery stenting for a two-vessel lesion. We further noted this. The main basic characteristics are presented in Table 1. Also in one of the cases, according to CT angiography, there was the filling of the right renal artery from the aortic false lumen (case presentation).
|
Table 1. Baseline characteristics |
||
|
Characteristics |
Number (n=9) |
% |
|
Mean age |
71.2 (5.8) years |
|
|
Female |
5 |
55.6 |
|
Chest pain at presentation |
7 |
77.8 |
|
Diabetes mellitus |
1 |
11.1 |
|
Hypertension |
8 |
88.9 |
|
Smoking |
4 |
44.4 |
|
Hypercholesterolemia |
6 |
66.7 |
|
Congestive heart disease presentation |
7 |
77.8 |
|
Glomerular filtration rate (MDRD) |
73.8 (21.4) ml/min/173 m2 |
|
|
Hemoglobin |
138.7 (28.9) g/l |
|
Technique of procedures
After clinical preparation and received consent, patients were transferred to catheterization laboratory. General anesthesia and intubation were applied. After clinical manifestations of coronary heart disease and presence of the indirect indications (age, hypercholesterolemia) established, the angiography of the coronary arteries was performed (radial approach). Then, the bifurcation of the common femoral artery was separated (at the right side in TEVAR, on both sides in EVAR). The artery was approximated by tourniquets. Puncture and the introducer insertion were performed above the bifurcation site. A pigtail catheter was inserted with the guidewire to the aortic root. Then superstiff or extrastiff guidewire was installed. For angiography, a second catheter was placed simultaneously through the radial approach above the proximal tear or the neck of the aneurysm. We performed short images for better positioning of the stent graft.
After successful placement, the delivery system was removed. A post-dilatation was done to the aortic balloon in the presence of incomplete placement or endoleaks. The puncture site and the wound were sutured and control was carried out regularly.
Endpoints
Full and correct placement of stent graft during implantation; postoperative absence of endoleaks; all-cause mortality, neurological, organs and extremities deficits, further dissection, expansion and absence of aneurysm thrombosis were included in the 6-month follow-up. The patients were also followed-up with echocardiography, ultrasound with Doppler and CT angiography.
Statistical analysis:
We used descriptive statistics to present data.
Results
Thoracic endovascular aortic repair (TEVAR) was done in eight cases with one endovascular aneurysm repair (EVAR) performed. According to the angiography, two patients had significant lesions of the coronary arteries. Among patients who underwent TEVAR, 3 (33%) had a concomitant thrombosed infrarenal aneurysm.
As a result of the analysis, we obtained satisfactory outcomes. All patients reached the 6-month endpoint. We have not recorded any aneurysm expansion, lack of aneurysm thrombosis or a functioning false lumen at the sites of the stent graft implantation. In addition, no further progression of the false lumen below the implantation zones was visualized. Mean diameter of stent grafts was 31.4 (4.8) mm and is 188.9 (34.6) mm in length. Valiant Thoracic Stent Graft with the Captivia Delivery System/ Endurant II Stent Graft System (Medtronic, Ireland) and Seal Thoracic Stent Graft (S&G Biotech, South Korea) were used. All patients underwent full deployment of the stents graft. One patient underwent additional balloon adjustment due to the presence of endoleak III.
Two patients (22.2%) had the procedure with left subclavian arteries overlapping. One patient had a filling of the right renal artery from the false lumen before the procedure. There was no 6-month examination based evidence of neurological, organs and extremities deficits.
Case report
Patient U., 53 years old male was admitted with suspicion of acute coronary syndrome. After the necessary studies, coronary angiography, CT angiography revealed acute aortic syndrome (thoracic aortic aneurysm and dissection to the right common iliac artery: entrance tear at the left subclavian artery (LSA) orifice, secondary tears near renal and superior mesenteric arteries, and the right renal artery was filled from the false lumen. EF–33%; Hb–144g/l; serum creatinine-119mcm/l. The patient had longstanding hypertension (max. 300 mm Hg) and congestive heart failure. The patient was receiving therapy for controlled hypotension. After preparation, stent graft was implanted Valiant Thoracic Stent Graft with the Captivia Delivery System (Medtronic, Ireland) with overlapping of LSA. After 6 month, CT angiography was showing thrombosed false lumen (Fig. 1) in stent graft zone and functioning distal fenestra. Doppler showed satisfactory blood flow velocity on LSA and right renal artery.
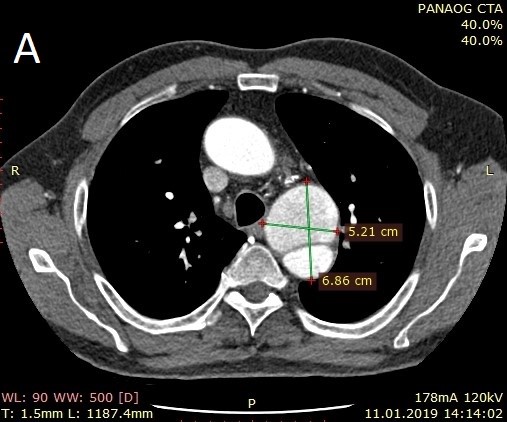
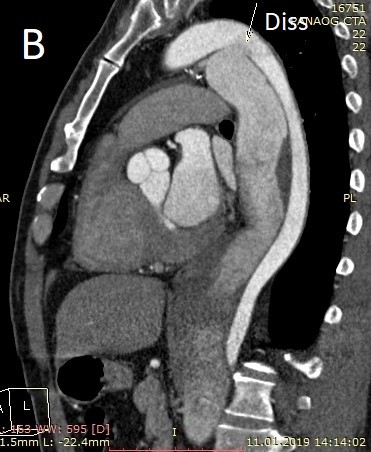

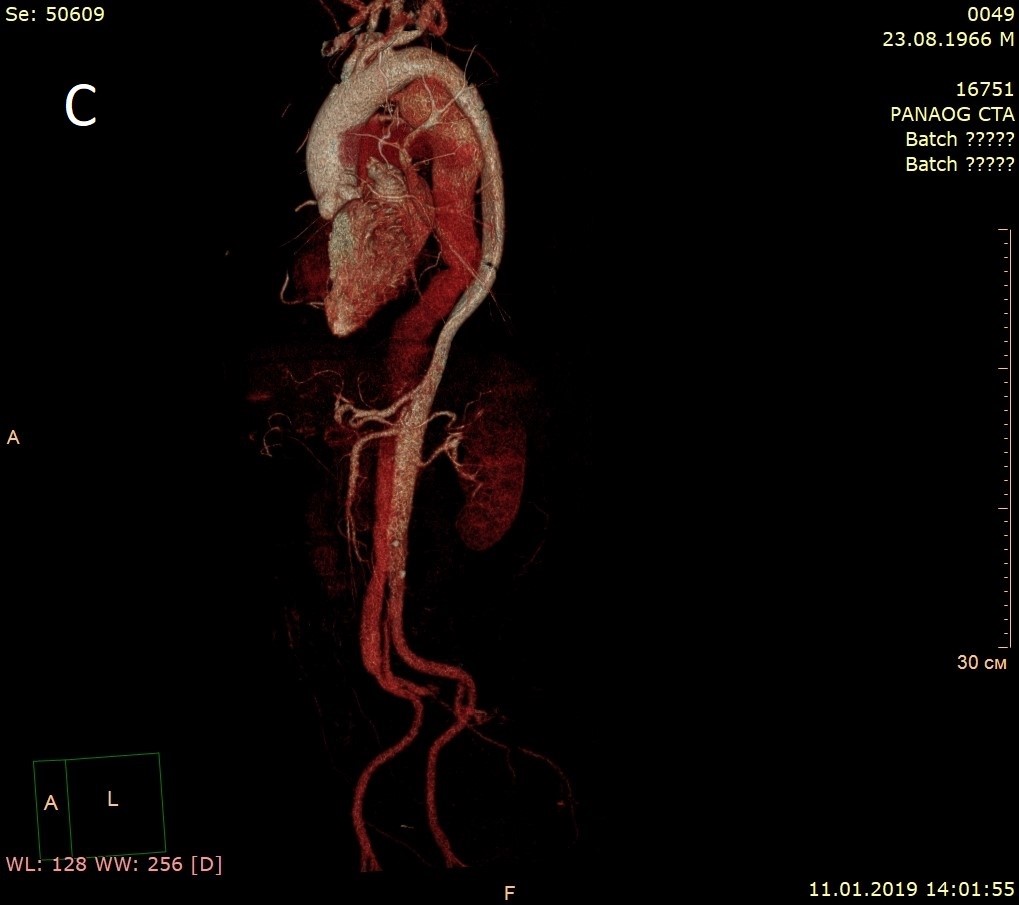
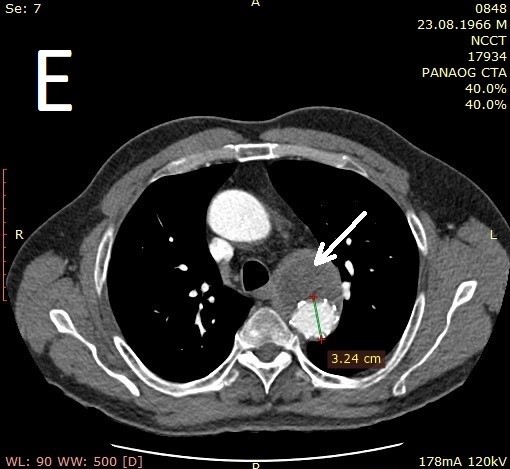
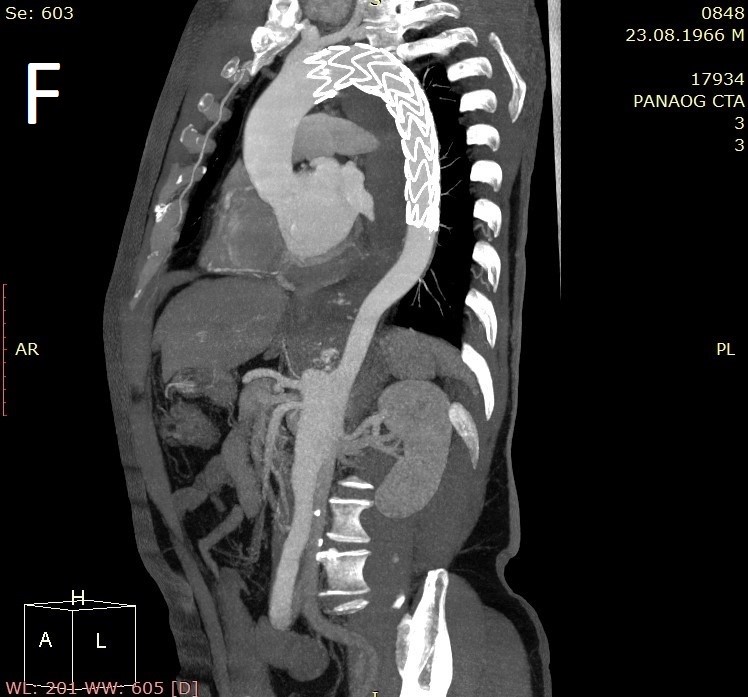


Figure 1. А, B - thoracic aortic aneurysm and dissection (arrow); C – common aortic 3D view; D – originate of renal arteries; E – implanted stent graft (arrow is pointing to thrombosed false lumen; F – implanted stent graft in section; G – lower tear (mesenteric zone); H - origination of renal arteries (right from false).
Discussion
Despite the lack of necessary circumstances for the development and implementation of stent grafts implantation procedures in Kyrgyzstan, it still can be done. In many ways, this procedure remains non - alternative method to prevent adverse events. Severe comorbidity, localization of aneurysms in the thoracic aorta, long distal dissection, and the hazard of the open intervention necessitate a greater consideration of the TEVAR and EVAR procedures.
Survival of patients with thoracic aorta aneurysm in the natural course of the disease (no surgery) can be represented as follows: 65% - within 1 year; 36% - for 3 years; 20% - for 5 years (11). AA dissection and its rupture with bleeding into the pericardial or pleural cavity are complications of an aortic aneurysm. The main reason for dissecting aortic aneurysms is arterial hypertension (12-14). Studies suggest an incidence of 2.6 to 3.5 cases per 100 000 person-years. In a review of 464 patients from the International Registry of Acute Aortic Dissection (IRAD), two thirds were male, with a mean age of all patients as old as 63 years. Although less frequently affected by acute aortic dissection, women were significantly older than men, with a mean age of 67 years (15). There are many risk conditions for aortic dissection. The most common predisposing factor in IRAD is hypertension (72%). A history of atherosclerosis was present in 31% and a history of cardiac surgery in 18%. In the total registry, 5% and 4% of acute aortic dissections were thought to be related to Marfan’s syndrome and iatrogenic causes, respectively. Traumatic aortic injury (TAI) also is a life-threatening condition that requires prompt diagnosis and management. It accounts for many cases. It is estimated that aortic injuries are lethal in 80-90% of cases (16). Thirty-two percent of patients with type A AAS were aged >70 years. Fewer elderly than younger patients were managed surgically (64 versus 86%; p<0.0001). In-hospital mortality was higher among older patients (43 versus 28%; p=0.0006). Logistic regression analysis identified age >70 years as an independent predictor of hospital death for acute type A dissection. In general, mortality from aortic dissection remains from 10.5% (type B) to 32.5% (Type A) (17-19). Analysis of the young patients with dissection (less 40 years of age) revealed that younger patients were less likely to have a history of hypertension (34%) or atherosclerosis (1%) but were more likely to have Marfan’s syndrome, bicuspid aortic valve, and/or prior to aortic surgery (20). Based on our observations the majority of patients also had high blood pressure. In addition no deaths were recorded, which can change with the further enrollment of patients.
The most significant rupture risk predictor is the size of the aneurysm. The critical diameter of the TAA, at which the risk of rupture and dissection sharply increases, is 6.0-cm. The risk factor for TAA rupture, related to its size, is the growth rate of the aneurysm. The average TAA progression rate is 0.1 cm per year, for TAA with chronic dissection varies from 0.24 cm per year for small aneurysms (4.0 cm) to 0.48 cm per year for large aneurysms (8.0 cm) (21).
As a rule, the identification of life-threatening conditions of the aorta at the stage of uncomplicated aneurysms, requiring a drug-based approach, is small and random. This represents a huge challenge. Most often, patients are hospitalized with complications, such as dissection. Obvious is the necessity to inform patients about successful stent grafts implantations experience, the creation of logistics and adding to national guidelines.
Conclusion
This modest observation showed the effectiveness of stent grafts implantation procedures in various aortic life-threatening conditions, such as aneurysm and / or aortic intima dissection. It is necessary to increase the number of patients, the follow - up period and the further development of this method in the Kyrgyz Republic.
Conflict of interest: None to declare
Authorship: A.I.Z., Ch. S. D., A.M.A., B. I.H., Ch.M. A., Ch. D. Ch., N. K.N, D. B.S. equally contributed to the study and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

