From Editor-in-Chief: Our progress and visibility, current issue, news from AHA 2024, trials and new guidelines, long COVID and welcome to new Editors
EDITORIALS
From Editor-in-Chief: Our progress and visibility, current issue, news from AHA 2024, trials and new guidelines, long COVID and welcome to new Editors
Article Summary
- DOI: 10.24969/hvt.2024.529
- CARDIOVASCULAR DISEASES
- Published: 11/12/2024
- Received: 09/09/2024
- Accepted: 09/09/2024
- Views: 3286
- Downloads: 2273
- Keywords: editorial
Address for Correspondence: Gulmira Kudaiberdieva, Editor-in-Chief, Heart, Vessels and Transplantation
E-mail: editor@hvt-journal.com

From Editor-in-Chief: Our progress and visibility, current issue, news from AHA 2024, trials and new guidelines, long COVID and welcome to new Editors
Dear readers
First of all, wish you happy holiday season and a very healthy, happy and successful New Year. We will acknowledge the authors of the most read articles on our website, on social media and most cited articles, outstanding reviewers in January 2025, and provide certificates, once we will have all required statistics for year 2024 at the beginning of January 2025.
I continue updating our scientific performance as a journal.
For past quarter, since September issue more our articles have been cited constituting 30% of our SCOPUS indexed content and we have gained 100 citations (Fig. 1). Our Hirsch index is 4 on SCOPUS and Google Scholar H5 index is 5 and H5 median index is 7 (1, 2). We should acknowledge our percentile in SCOPUS for transplantation is increased from 2% to 4% (1).
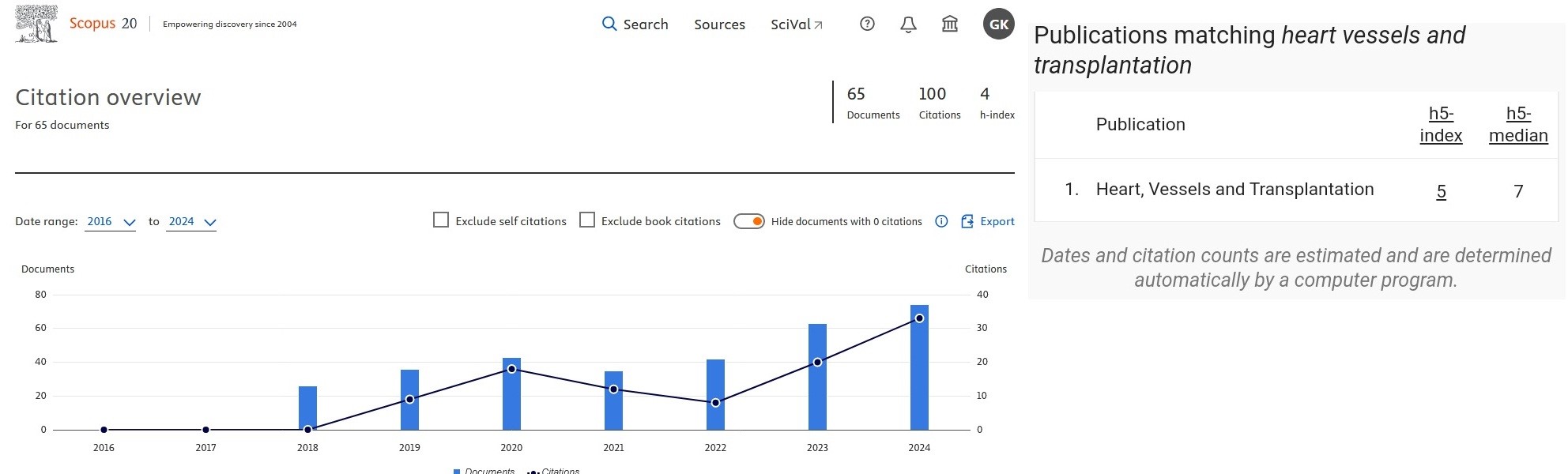
Figure 1. SCOPUS Hirsch index, number of citations and cited documents (left ) and Google scholar metrics (right) panel by December 2024 for Heart, Vessels and Transplantation (2, 3)
We have to acknowledge the following important statistics that SCIMAGO database (3) (Fig. 2) provided: in 2023 our number of women authors reduced from 50% in 2018 to 28.96% in 2018, that might be related to geographical expansion of our authors, that correlates with our readers - for example our Facebook female followers constitute only 25% (Facebook followers are from 147 countries).
However, number of articles related to the UN The Sustainability Development Goals on good health and well-being (4) increased from 4 in 2018 to 28 in 2023. This means that we increased number of articles regarding prevention, promoting health in area of cardiovascular health (5), public health, health policies and pandemics and health environment (6). This includes our research, review articles and Editorials.
We keep our diversity as International collaboration pear article in 2023 shows that 4.76 countries collaborated per article (3).
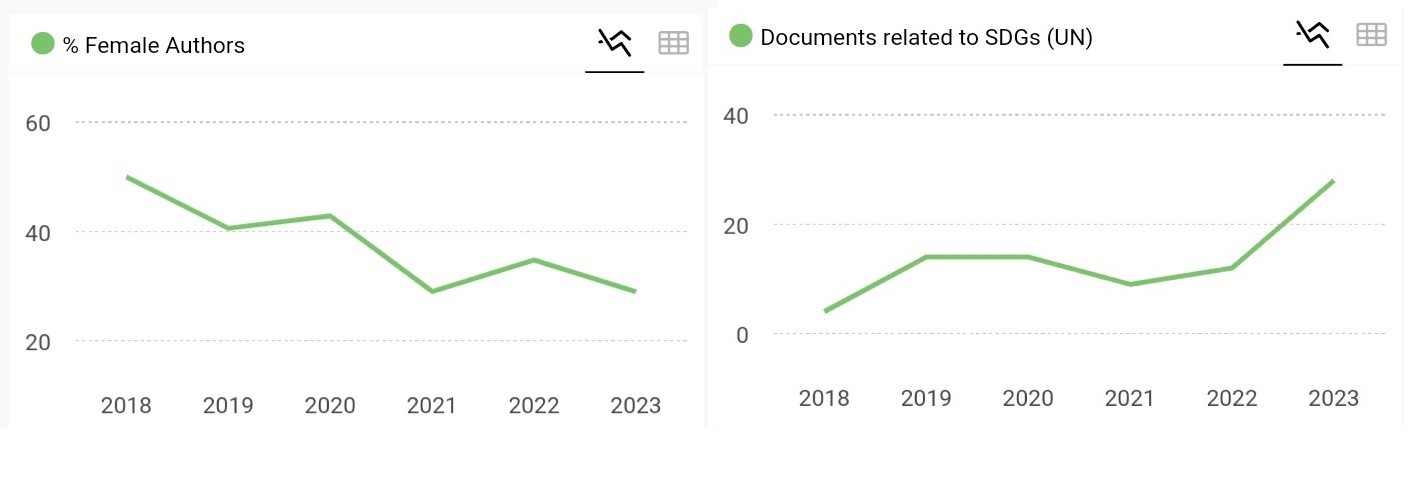
Figure 2. Dynamics of female authors (left) and articles in frame of UN Sustainable Development Goals (right) for the period of 2018 and 2023 for Heart, Vessels and Transplantation journal, SCIMAGOJR analytics (3)
Interesting new statistics we have for our website – our readers from 41 countries of 207 total accessed our website using artificial intelligence (AI) (LLM - ChatGPT and others). It will be interesting to know whether AI impacts citations, as AI programs are being used for literature search, writing and generating images. As we know twitter activity increases chance being cited by 2.7 times (95%CI 2.12.-3.8, p< 0.001), this is adjusted for IF, meaning that higher impact factor journals have larger audience (4). I have to remind all authors who use AI that they are obliged to disclose use of AI in preparation of manuscripts and confirm they critically reviewed content, as AI LLM is a developing tool and errors may occur (5).
Current issue includes editorials introducing the 2024 ESC guidelines on stable coronary heart disease, elevated blood pressure and hypertension, and peripheral arterial and aortic diseases prepared by our Editors and invited experts; research articles and meta-analysis of importance for you – on renal dysfunction in patients with acute coronary syndromes and heart failure with preserved ejection fraction (HFpEF) and its effect on outcomes; on association of simple laboratory tool as neutrophil- albumin ratio with the risk of aortic valve sclerosis; role of PUMA score in detection of patients with chronic obstructive pulmonary disease, important for healthcare facilities without pulmonary function test capabilities; on outcomes of surgery for anomaly of abdominal wall – gastroschisis in newborns, as this anomaly is also accompanied by congenital heart defects; on iatrogenic right atrial thrombosis secondary to central venous catheter use and hemodialysis; renal tissue oximetry in prediction of acute kidney injury in infants undergoing cardiac surgery; experimental study on the effect of exclusively fat diet on brain vasculature; and study on association of training type and training duration with cardiac remodeling in female athletes; meta-analysis on transcatheter versus surgical aortic valve replacement outcomes in low-to- intermediate risk of severe aortic stenosis patients.
Interesting case reports: on successful Bentall-Bono procedure with biological aortic valve replacement in patents with bicuspid valve stenosis and aortic root pathology; long term outcome of hybrid treatment of saccular aneurysm of aortic arch using carotid-carotid-subclavian artery bypass and stent graft of aneurysm; a rare case of cardiac angiosarcoma presented as massive pericardial effusion and successful surgery; a case of successful treatment of isthmus dependent atrial flutter with left atrial activation sequence, diagnosed without transseptal puncture and severe infective endocarditis developed after abdominal surgery and temporary venous lines.
Three ESC 2024 guidelines are introduced by our editors in this issue and I would like shortly mention atrial fibrillation (AF) 2024 ESC (9) and EACTS 2024 consensus papers and guidelines (10- 12). They will be introduced by our Editors and experts in coming issues.
AF 2024 guidelines (9) is based on a patient care approach. Clinical AF is defined as asymptomatic and symptomatic arrhythmia documented by 12 lead electrocardiogarm (ECG) or ECG devices. Definition of AF on temporal basis includes: first-diagnosed, paroxysmal, persistent and permanent. The guideline introduces patient CARE approach: (C) the risk factor and comorbidities management, (A) avoid stroke and thromboembolism, (R) reduce symptoms by rate and rhythm control and (E) evaluation and dynamic measurement. For A – the risk of thromboembolism and bleeding should be assessed and most patients should receive direct oral anticoagulants. R - rhythm control - use electrical cardioversion as class I for patients with hemodynamic instability (green) and consider waiting 48 hours for spontaneous cardioversion in patients without hemodynamic instability - class IIa recommendation (yellow) or consider electrical or pharmacological cardioversion for symptomatic persistent AF patients (yellow), see other yellow and red recommendations in guidelines. For pharmacological cardioversion – use (green) flecainide and propafenone for recent onset AF without HF with reduced ejection fraction (HFrEF), coronary artery disease (CAD) of left ventricular hypertrophy (LVH). For patients with AF and recent onset iv vernacalant is recommended in absence of HFrEF, CAD and severe aortic stenosis. Amiodarone as an agent for pharmacological conversion is recommended for patients with AF and LVH, HFrEF and CAD. Catheter ablation is recommended for patients paroxysmal or persistent AF resistant to antiarrhythmic drug therapy (AAD) or as first=line therapy is recommended after shared decision- making in AF patients to reduce symptoms, progression and recurrence of AF. Ablation is also recommended for patients with AF and HFrEF with tachycardia induced cardiomyopathy to reverse ventricular dysfunction. Endoscopic and hybrid AF ablation (yellow recommendation) should be considered in patients with symptomatic resistant to AAD persistent AF as decision- shared strategy between electrophysiologists and surgeons to reduce symptoms, progression and recurrence of AF. Concomitant surgical ablation is recommended in patients with AF and mitral valve disease. Oral anticoagulation recommendations accompany all rhythm control strategies. Left atrial appendage (LAA) occlusion is recommended (green) to prevent thromboembolism in patients with AF patients undergoing cardiac surgery, should be considered (yellow) in those undergoing hybrid and endoscopic AF ablation and may be considered in patients with contraindication to OAC (orange). See details for yellow and orange and red in guidelines. There are patient care pathways for first-diagnosed, paroxysmal, persistent and permanent AF.
I recommend for Heart teams (cardiac surgeons, anesthesiologists and reanimatologists, perfusiologists, cardiologists and imaging and laboratory specialists) managing patients undergoing cardiac surgery to read and implement in clinical practice the following EACTS guidelines published in 2024 – EACTS consensus paper on acute myocardial infarction (AMI) after cardiac surgery (10), EACTS cardiac surgery guidelines on blood management (11) and perioperative medications guidelines (12).
Consensus paper on perioperative myocardial infarction (PMI) after cardiac surgery (10) defines strategy for diagnosis of injury and AMI after cardiac surgery based on biomarker levels and supportive ECG signs of ischemia/infarction, angiographic (coronary angiography, computed tomography angiography or cardiac magnetic resonance (CMR) imaging documentation of graft or coronary artery occlusion) and imaging (transthoracic or transesophageal echocardiography or positron emission tomography, CMR signs of regional wall abnormalities or loss of viable myocardium) sign. If hsTn is ≥10 times higher 99th upper reference level (URL) repeat 24 hours after surgery and if level is ≥35 10x99% URL and supportive signs of ischemia/AMI – PMI; if no elevation ≥35 10x99%URL and no supportive evidence of ischemia- it is a perioperative biomarker elevation. And if only elevation ≥35 10x99%URL – perioperative myocardial injury.
If there is an increase in hsTn ≥35-500 10x 99%URL and supportive signs of ischemia - PMI and if no supportive ischemia/ AMI signs and repeated test 24 hours after surgery is ≥500 10x99%URL– PMI, if not then- perioperative myocardial injury . If hsTn- is ≥500 10x99%URL– PMI.
The EACTS blood management guidelines (11) endorse multidisciplinary approach in management of patients undergoing cardiac surgery starting with prior admission – medical history, physical examination, bleeding history, determining risk of bleeding, diagnosing anemia, laboratory tests as complete blood count and coagulation tests; preoperative – identification of patients at high risk of bleeding, guideline-directed management of antithrombotic medications, platelet function testing in patients on dual antiplatelet therapy (DAPT), and fibrinogen level testing; intraoperative – manage hemostasis and minimize blood loss; minimize hemodilution optimizing cardiopulmonary bypass (CPB), ultrafiltration and autologous priming, identification of anemia and its treatment, maintenance of normothermia and Ph, management of heparin and protamine doses, prevention of fibrinolysis and cell salvage; postoperative – use point of care algorithms for bleeding patients; fibrinogen supplementation for bleeding patients with low fibrinogen <1.5 g/l , identification of anemia and treatment, prothrombin complex concentrate and fresh frozen plasma for bleeding patients with coagulation factor deficiency, platelet transfusion for bleeding patient with platelet count <50 x109/L and or desmopressin and platelet transfusion, packed red blood cell of all ages restrictive transfusion triggers, and early re-exploration. The new guidelines now describe in detail anemia included management and detailed CPB techniques, intravascular and anticoagulation management; postoperative chest tube drainage management, re-exploration, postoperative transfusion triggers and resumption of antithrombotic therapy and venous thromboembolism prophylaxis.
The EACTS guidelines on medication management (12) in patients undergoing cardiac surgery endorse also multidisciplinary approach on preoperative, intraoperative and postoperative management including all spectrum of medications - cardiovascular, antithrombotics, infection control, etc, The main messages are: it is recommended (green) to: continue beta-blockers, calcium-channel blockers and administer gastroprotective medication preoperatively; continue acetylsalicylic acid perioperatively; switch from vitamin K antagonist (VKA) to heparin or low molecular weight heparin in patients with high thrombotic risk; prescribe mupirocin intranasally 4 days before surgery to prevent S.aureus infection; use antibiotic prophylaxis one hour before skin incision; resume or start DAPT after surgery for patients with history of ACS and percutaneous coronary intervention; use VKA with international ratio (INR) monitoring training in patients with mechanical prosthetic heart valves and use VKA for 3 months after bioprosthetic valve implantation in patients with mitral and tricuspid valve disease, use oral anticoagulation therapy for 4 weeks in patients with persistent postoperative atrial fibrillation (POAF); use long-term and optimal renin-aldosterone- angiotensin- system inhibition for patients with heart failure HF or hypertension, use life-long cadioselective beta-blockers and sodium glucose co-transporter inhibitor in HFrEF. There are also considered to do recommendations (yellow) – see guidelines for specific situations and conditions when and to whom apply theses recommendation and red – contraindicated – not recommended recommendations.
We keep our hand on pulse of major meetings. The AHA annual sessions took place in November 2024 in Chicago, Illinois, USA. The most important trials that attract my attention are MHYH, VANISH2, OPTION, CLEAR, SUMMIT, and several others. The are 2 negative trials in AMI patients. CLEAR investigators demonstrated absence of benefit of colchicine as anti-inflammatory agent in AMI (13) with no reduction of composite event as death, stroke, coronary revascularization, however diarrhea occurred in significantly more frequently colchicine group. The 2nd arm of CLEAR trial revealed no effect of mineral corticoid aldosterone (MRA) inhibitor spironolactone in AMI patients without HF in terms of mortality, re-infarction and rehospitalizations (14). We do not use spironolactone in patients with AMI without HF and await more evidence to fight the inflammation in AMI.
On the other hand, in HF patients FINEARTS-HF trial tested hypothesis whether nonsteroidal MRA finerenone (20 to 40 mg) has different effect on primary composite outcome (cardiovascular death and any HF event) between women (n=2732) and men (n=3269) with mildly reduced or preserved ejection fraction (<40%). Authors did not find any difference in the risk of composite outcome development between both sexes (HR 0. 78 for women and 0.88 for men).
This trial showed no sex specific difference to nonsteroidal MRA treatment, while previous studies showed better outcome for women on steroidal MRA and sacubitril/valsartan (ARNI) (15).
Another obesity drug, is shown to effectively reduce cardiovascular death rate, worsening of HF and improve quality of life in patients with HFpEF – tirzepatide long-acting agonist of glucose-dependent and insulinotropic polypeptide and glucagone –like peptide receptor 1 (16).
Good news for chemotherapy cardiotoxicity prevention in patients with cancer. SARAH trial demonstrated that ARNI –use in patients with cancer undergoing chemotherapy with anthracycline reduced relative risk of cardiac toxicity and injury by 77%. There was improvement in global longitudinal strain in ARNI group as compared to its worsening in placebo group (17).
For myosin inhibitor approved for treatment of hypertrophic cardiomyopathy (HCM), there were concerns regarding HFrEF development. The live registry study on mavacamten the cardiac myosin inhibitor demonstrated the low incidence of ejection fraction reduction <50% in cohort of patients with HCM – of 5573 patients EF reduction in requiring hospitalization for HFrEF was 1.3%. The need of treatment interruption was low. And the left ventricular outflow gradient reduced <30 mmHG in 70% of patients after 6 months of therapy (18).
There are several important trials in the area of arrhythmias and electrophysiology that might contribute to the guidelines updates on AF and VT.
The pCAD-POAF randomized controlled trial tested effect of removal of epicardial adipose tissue and cutting Marshall ligament with resection of fat pad along the Waterstone groove - cardiac autonomic nervous system morphological elements, on POAF development in patients without history of AF undergoing coronary bypass surgery (CABG). Authors demonstrated 47% decrease in risk of AF after surgery (RR - 0.57 95%CI 0.41-0.81) (19).
VANISH2 trial compared 2 strategies as initial therapy in patients with ischemic cardiomyopathy and ventricular tachycardia (VT): catheter ablation and antiarrhythmic drug (amiodarone and sotalol) therapy. Authors demonstrated 25% reduced risk (HR- 0.75, 95% CI 0.58-0.97, p=0.03) of composite event (death of all causes, electrical storm, ICD appropriate shock or antitachycardia pacing, sustained VT requiring termination in emergency department) during 4.3 years of follow-up in catheter ablation group as compared to drug therapy. Adverse effects were often in drug arm (20).
OPTION trial evaluated effect of LAA closure on bleeding and primary and secondary efficacy endpoints in patients with AF undergoing catheter ablation with high risk of embolic events (CHA2DS2Vasc score ≥2 in men and ≥3 in women). Patient were randomized to LAA closure (803) and anticoagulant treatment (797) after catheter ablation and were followed up for 36 months for development of primary safety endpoint - non-procedure related major bleeding, primary efficacy end-point - composite outcome (death, stroke or systemic embolism) or secondary efficacy end-point - procedure related bleeding. Non-procedure related bleeding developed in significantly less patients with device as compared to drug therapy (8.5 vs 18.1%, p<0.001), as well as death, stroke and embolism and procedure related bleeding were lower (p<0.001 for both).Thus this trial showed superiority of LAA closure over drugs for major bleeding and non-inferiority in terms of procedure related bleeding and efficacy outcomes as compared to anticoagulation (21).
The My Heart Your Heart trial test the risk of infection and device failure with use of reconditioned permanent pacemakers (PPM) (decontamination, set screw, screw cap replacement and electrical testing and sterilization) in patients with class 1 indications for PPM implantation and no financial means as compared to patients with new devices. Study was performed in low income countries. During 1- year follow-up the infection developed in reconditioned group in 1.5% vs 2.9% in new device group, lead dislodgement in 7.3% vs 5.0% and death in 2.2% vs 0%, respectively. Of all patients with preconditioned PPM 79% had complete atrioventricular block and 25% - sinus node dysfunction. Time to infection was longer and lead dislodgement was slightly higher in reconditioned PPM as compared to new device. Promising results to save lives for populations without financial means (22).
Good news for tricuspid valve transcatheter edge- to- edge repair (T-TEER). Randomized clinical trial (23) demonstrated that T-TEER reduced by 16% 2- year all-cause mortality, though not significantly as compared to surgery. However T-TEER patients had lower postoperative in-hospital mortality (2.5 vs 12.5%, p<0.001) and permanent pacemaker implantation rate (0% vs 12.7%, p<0.001) as compared to surgery group.
And keep an eye on live updating knowledge on long COVID, as you can face its various manifestations in your patients (24).
I would like to welcome our new Editor – Aditya Sood from Conway, NC, USA. She joined our International Editorial Board as Editor on cardiovascular imaging (echocardiography, cardiac computed tomography, cardiac magnetic resonance imaging and nuclear imaging). We look forward for our successful cooperation in evaluating and selecting best evidence.
Gulmira Kudaiberdieva
Editor-in-Chief
Heart, Vessels and Transplantation
Peer-review: Internal
Conflict of interest: None to declare
Authorship: G.K.
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: We declare that we did not use AI-assisted technologies in preparation of this manuscript
References
| 1.Scopus sources. Available at: URL: https://scopus.com/sources | ||||
| 2. Google scholar. Available at: URL: https://scholar.google.com/citations | ||||
| 3. SCImago journal & country rank. Available at: URL: https://www.scimagojr.com | ||||
| 4. United Nations. Sustainable development. 3, Ensure healthy lives and promote well-being for all at all ages. Available at: URL: https:// sdgs.un.org/goals/goal3 | ||||
| 5.Zoghbi WA, Duncan T, Antman E, Barbosa M, Champagne B, Chen D, et al. Sustainable development goals and the future of cardiovascular health: a statement from the Global Cardiovascular Disease Taskforce. J Am Coll Cardool 2014; 64: 1385-7. https://doi.org/10.1016/j.jacc.2014.08.018 PMid:25257641 |
||||
| 6. WHO. Sustainable development. Available at URL: https://who.int/healh-topics/ sustainable-development | ||||
| 7. Sousa JA, Alves IA, Donato H, Freitas JS. The twitter factor: How does Twitter impact Stroke joiurnals and citation rates. Int J Stroke 2023; 18: 586-9. https://doi.org/10.1177/17474930221136704 PMid:36285888 |
||||
| 8. Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals. Updated January 2024 Available at: URL: www.icmje.org. Accessed on 9.02.2024 | ||||
| 9. Van Gelder IC, Michiel Rienstra M, Bunting KV, Casado-Arroyo R, Caso V, Crijns HJGM, et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2024; 00: 1-101. Doi: 10.1093/eurheartj/ehae176 https://doi.org/10.1093/eurheartj/ehae176 PMid:39210723 |
||||
| 10. 10. Gaudino M, Flather M, Capodanno D, Milojevic M, Bhatt DL, Milojevoc M, et al. European Association of Cardio-ThoracicSurgery (EACTS) expert consensus statement on perioperative myocardial infarction after cardiac surgery. Eur J Cardiothorac Surg 2024; doi:10.1093/ejcts/ezad415 https://doi.org/10.1093/ejcts/ezad415 PMid:38420786 |
||||
| 11. Casselman FPA, Lance MD, Ahmed A, Ascarie A, Blanco-Morillof J, Bolligerg D, et al. 2024 EBCP. | ||||
| EACTS/EACTAIC/EBCP Scientific Document Group. | ||||
| EACTS/EACTAIC Guidelines on patient blood management in adult cardiac surgery in collaboration with EBCP. Eur J Cardtiothorac Surg 2024; doi: 10.1093/ejcts/ezae352/7815985 | ||||
| 12. Jeppsson A, Rocca B, Emma C. Hansson EC, Gudbjartsson T, James S, et al. EACTS Scientific Document Group.2024 EACTS Guidelines on perioperative medication in adult cardiac surgery. Eur J Cardtiothorac Surg 2024; doi: 10.1093/ejcts/ezae355/7815986 https://doi.org/10.1093/ejcts/ezae355 PMid:39385505 |
||||
| 13. d'Entermont MA, Lee SF, Mian R, Tyrwhitt J, Kedev S, Montalesot J, et al. Colhicine in acute myocardial infarction. N Engl J Med 2024;doi: 10.1056 /NEJMoa2405922 | ||||
| 14. Jolly SS, d'Entermont MA, Lee SF, Mian R, Tyrwhitt J, Kedev S, et al. Routine spironolactone in acute myocardial infarction. N Engl J Med 2024;doi: 10.1056 /NEJMoa2405923 https://doi.org/10.1056/NEJMoa2405923 PMid:39555814 |
||||
| 15.Chimura M, Wang X, Jhund PS, Henderson AD, Claggett BL. Desai AS, et al. Finerenone in women and menwith heart failure with mildly reduced or preserved ejection fraction. A secondary analysis FINEARTS -HF Randmized Clinical Trial. JAMA CArdiol 2024; doi:10.1001/jamacardio.2024.4613 https://doi.org/10.1001/jamacardio.2024.4613 PMid:39550721 PMCid:PMC11571069 |
||||
| 16. Packer M, Zile MR, Baum SJ, Litwin SE, Ge J, et al. Tirzepatide for heart failure with preserved ejection fraction and obesity. N Engl J Med 2024;doi: 10.1056 /NEJMoa2410027. https://doi.org/10.1056/NEJMoa2410027 PMid:39555826 |
||||
| 17. Bonato MC. Effects of sacubitril/vaslartanon preention of cardiotoxicity in high-risk patients undergoing anthracycline chemotherapy. American Heart Association. AHA 2024 annual Scientific Session, Chicago, Illinois, November 18. | ||||
| 18. Desai MY, Seto D, Cheung M, Afsari S, Patel N, BAstien A, et al. MAvacamten real-world exepriemce from 22 months of the risk evaluation and mitigation strategy *(REMS) program. Circulation: Heart Fail 2024; doi: 10.1161./CICHEARTFAILURE.124.012441 https://doi.org/10.1161/CIRCHEARTFAILURE.124.012441 PMid:39523955 |
||||
| 19. Yang Z, Tiemuerniyazi X, Xu F, Wang Y, Sun Y, Yan P. Partial cardiac denervationto prevent postoperative atrial fibrillationafter coronary artery bypass grafting. The pCAD-POAF randomized clinical trial. JAMA CArdiol 2024; doi:10.1001/jamacardio.2024.4639 https://doi.org/10.1001/jamacardio.2024.4639 PMCid:PMC11571071 |
||||
| 20. Sapp J, Tang ASL, Parkash R, Stevenson WG, Healey JS, Gula LJ, et al. Catheter ablation or antiarrhythmic drugs for ventricular tachycardia. N Engl J Med 2024;doi: 10.1056 /NEJMoa2409501 | ||||
| 21. Wazni QM, Saliba WI, Nair DG, MArijon E, Schmidt B, Hounshell T, et al. Left atrila appendage closure after ablation for atrial fibrillation. (N Engl J Med 2024;doi: 10.1056 /NEJMoa2408308 https://doi.org/10.1056/NEJMoa2408308 PMid:39555822 |
||||
| 22. Crawford T. Preliminary results of randomized trila of new versus reconditioned pacemakers for pateinst unable to obtaina new device in low low medium income countries: The My Heart Your Heart (MHYH) randomized trial. American Heart Association. AHA 2024 annual Scientific Session, Chicago, Illinois, November 17. | ||||
| 23. Shimoda T, Uyeama H, Myamoto Y, Watanabe A, Gotanda H, Kolte D, et al. Comparison of transcatheter versus surgical reapir among patients with tricuspid regurgitation: Two-year results. Circulation: Cardiovasc Interv 2024; doi: 10.1161/CIRCINTERVENTIONS.124.014825 https://doi.org/10.1161/CIRCINTERVENTIONS.124.014825 PMid:39556351 |
||||
| 24.CDC. Clinical overview of long COVID. Available at: URL: https:// www.cdc.gov/covid/hcp/clinical-overview/index.html | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

